Course Detail
Advanced Immunology
List of Contents
- General Introduction
- Innate Immunity
- Acquired Immunity
- Antigens
- Antibodies
- Antigen Antibody Reactions
- Humoral Immunity
- Cell Mediated Immunity (CMI)
- Lymphoid Organs and Tissues
- Types of Immune Cells
- The Major Histocompatibility Complex (MHC)
- Immunodeficiency
- Hypersensitivity
- Anaphylaxis
- Autoimmunity
- Transplant Immunology
- Tumor Immunology
General Introduction
Immunology is a branch of biology focusing on the physical, chemical and physiological characteristics of the immune system. This immunology course is sandwiched here between other microbiology courses, because the immune system is the body's response to invasion by pathogens and other foreign substances.
Classical immunology studies the relationship between body systems, pathogens and immunity.
Clinical Immunology is the study of diseases caused by disorders of the immune system including immunodeficiencies and autoimmunity.
Developmental Immunology refers to the aspects of the immune system and immune response that are influenced by the age of the individual. For example, children are in a state of physiological immune deficiency because they haven't been exposed to many pathogens.
Ecoimmunity and behavioral immunity refers to the immune system and response in relation to the individual's environment and or behavior.
Reproductive Immunology refers to aspects of the immune response related to the reproductive system such as fetus acceptance. In some cases, disorders like these might result in infertility.
Immunotherapy is the use of various immune system components to treat diseases. A good example is the treatment of allergies.
Cancer Immunology is the study of the immune response to cancer cells and these dynamics can be used to develop cancer treatments and diagnostic tools.
The body's defense mechanisms can be divided into: (a) innate (natural) immunity and (b) acquired (adaptive) immunity.
Innate Immunity
Innate immunity is the resistance that an individual possesses by birth. Innate immunity may be classified into three types:
- Individual Immunity
- Racial Immunity
- Species Immunity
Individual immunity refers to the resistance to infection, which varies within different individuals in the same race and species and is genetically determined. For example, if one homozygous twin develops tuberculosis, there is a very high possibility that the other twin will also develop tuberculosis. But in heterozygous twins, there is a very low possibility of the other twin suffering from tuberculosis.
Racial immunity: Racial immunity refers to differences in susceptibility or resistance to infection among different races within a same species. For example, races with sickle cell anemia prevalent in Mediterranean coast are immune to infection caused by malaria parasite Plasmodium falciparum.
Species immunity: Species immunity refers to a total or relative resistance to a pathogen shown by all members of a particular species. For example, chickens are resistant to anthrax while humans are susceptible.
Factors affecting Innate Immunity
Age: Extremes of age (very young or older individuals) are highly susceptible to various infections. Measles, mumps, poliomyelitis, and chicken pox are few examples of the diseases that cause more severe clinical illness in adults than in young children.
Nutritional status: Innate immunity is lowered in malnutrition.
Hormone levels: Individuals with certain hormonal disorders become increasingly susceptible to infection. For example, pregnant women are more susceptible to many infections due to higher level of steroid during pregnancy. Individuals suffering from diabetes mellitus, hypothyroidism, and adrenal dysfunction are more susceptible to staphylococcal and streptococcal infections.
Innate immunity is dependent on four types of defensive barriers:
- Anatomical barriers: Anatomic barriers include skin and mucous membrane. They are the most important components of innate immunity. They act as mechanical barriers and prevent entry of microorganisms into the body. The intact skin prevents entry of microorganisms. Mucous membranes form a most of the covering of hollow organs and systems. There are several nonspecific defense mechanisms that prevent entry of microorganisms through mucous membranes. For exmaple, Saliva, tears, and mucous secretions tend to wash away potential invading microorganisms preventing adhesion. These secretions also contain antimicrobial substances. Mucus is a viscous fluid secreted by the epithelial cells of mucous membranes. It helps to trap invading microorganisms. In the respiratory tract, the mucous membrane is covered with cilia, which are hair-like protrusions on the epithelial cell. The movement of cilia is coordinated so that it propels mucus entrapped microorganisms from these tracts towards the exterior or the body. Nonpathogenic organisms colonizing mucosal surfaces are called Normal Flora. They compete with pathogenic microbes for attachment sites on the epithelial cell surface and for necessary nutrients and reduce the development of infections.
- Physiological barriers: For example, the low pH in the stomach is an innate physiologic barrier to infection because very few ingested microorganisms can survive at that low pH. Other physiological barriers include lysozymes.
- Phagocytosis: Phagocytosis is a process of ingestion of extracellular particulate material by certain specialized cells, such as blood monocytes, neutrophils, and tissue macrophages.
- Inflammatory response: Tissue damage or the invasion by pathogenic microorganism induces a complex sequence of events, collectively known as the inflammatory responses. The four cardinal/typical characteristics of an inflammatory responses are rubor (redness), calor (rise in temperature), dolor (pain), and tumor (swelling). Histamine, kinins, acute phase proteins, and defensin are the important mediators of inflammatory reactions. Histamine binds to receptors on nearby capillaries and venules, causing vasodilatation and increased permeability. Typical signs observed during an allergic reaction.
Acquired Immunity
Adaptive Immunity can be classified into four kinds:
- Active Immunity
- Passive Immunity
- Herd Immunity
- Local Immunity
Active Immunity: Active immunity is the resistance developed by an individual after it comes into contact with foreign antigens such as microbes.
Active immunity can be categorised into two types
- Natural active immunity, which is acquired by natural clinical or subclinical infections. Natural active immunity lasts longer.
- Artificial active immunity, which is induced through vaccination
Passive Immunity: Passive immunity is achieved by transferring serum or lymphocytes from immunized individuals. The individuals develop resistance faster. Passive immunity may also be Natural or artificial. Natural passive immunity occurs when antibodies are transferred from the mother to her offspring during breast feeding. Artificial passive immunity is induced by the administration of antibodies in the form of antiserum raised against a specific pathogen.
Local Immunity: Immunity localized at a particular site such as the gut mucosa, nasal mucosa. uterus etc.
Herd Immunity: Herd Immunity (herd effect, community immunity, population immunity, or mass immunity) refers to a level of immunity that develops when a certain percentage of the individuals in a population have become immune to that pathogen either through vaccination or exposure to the pathogen. Immune individuals are unlikely to contribute to disease transmission, disrupting chains of infection, which stops or slows the spread of disease. Eradication of a disease relies on the development of a high herd immunity.
Antigens
The word antigen is short for Antibody generator. Aan antigen (Ag) is a molecule or molecular structure, that may be present on the outside of a pathogen, that can be bound by an antigen-specific antibody or B-cell antigen receptor.
Antigens are "targeted" by antibodies. Each antibody is specifically produced by the immune system to match an antigen after cells in the immune system have come into contact with it; this allows a precise identification or matching of the antigen and the initiation of an adaptive response.
On the other hand, Immunogens are molecules that induce an immune response. In most cases, antigens are immunogens, and the terms are used interchangeably. The antigens that are not immunogenic but can take part in immune reactions are termed as haptens. The term immunogenicity means the ability of an antigen to elicit an immune reaction in the form of a B-cell or T-cell response, whereas the term antigenicity means just the ability to combine specifically with the products of the above responses.
There are a number of factors that determine if a substance will be immunogenic. These include:
- Molecular size: larger molecular sizes are more antigenic. Substances with molecular weights of about 100,000 Da and more are highly immunogenic, while substances with molecular weights of less than 5000 Da are generally not immunogenic.
- Foreignness: Foreignness implies ability of the host to tolerate self-antigens. Tolerance to self-antigens develops by contact with them in the initial phases of the development of immune system, particularly during the development of lymphocytes. The more distant the species are, the greater the immunogenicity. For example, bovine serum albumin is more immunogenic in chicken than it is in goats.
- Chemical-structural complexity: Proteins and polysaccharides are more immunogenic. Nucleic acids are not immunogenic.
- Stability: Unstable substances are more immunogenic than stable substances.
Antigenic Specificity
The antigenic determinants are called epitopes. An epitope is defined as the immunologically active region of an immunogen that binds to antigen-specific membrane receptors on lymphocytes or secreted antibodies.
Species Specificity
Species possess soecies specific antigens that react with antigens from other species. Isoantigens are antigens found in some but not all members ofa species. In both cases, these antigens can be used to conduct phylogenetic studies.
Autospecificity: Proteins present in the cornea and sperms are not recognized as self antigens because they do not encounter the immune system during the development of tolerance. These tissues are immunogenic if they are exposed to blood or other tissues.
Organ specific antigens are proteins that are present in an individual but located in specific organis and cause an immune response if they are introduced into other organs. Brain-specific antigens are an example.
Antibodies
Antibodies are globulin protein molecules (thus also called Immunoglobulins). They are synthesized in serum and other body fluids. Antibodies react to specific antigens. The most important function is to confer protection against microbial pathogens. They achieve this function by:
Preventing attachment of microbes on mucosal surfaces of the host.
Reducing virulence of microbes.
Facilitating phagocytosis of microbes, and.
Activating the complement -mediated activities against microbes.
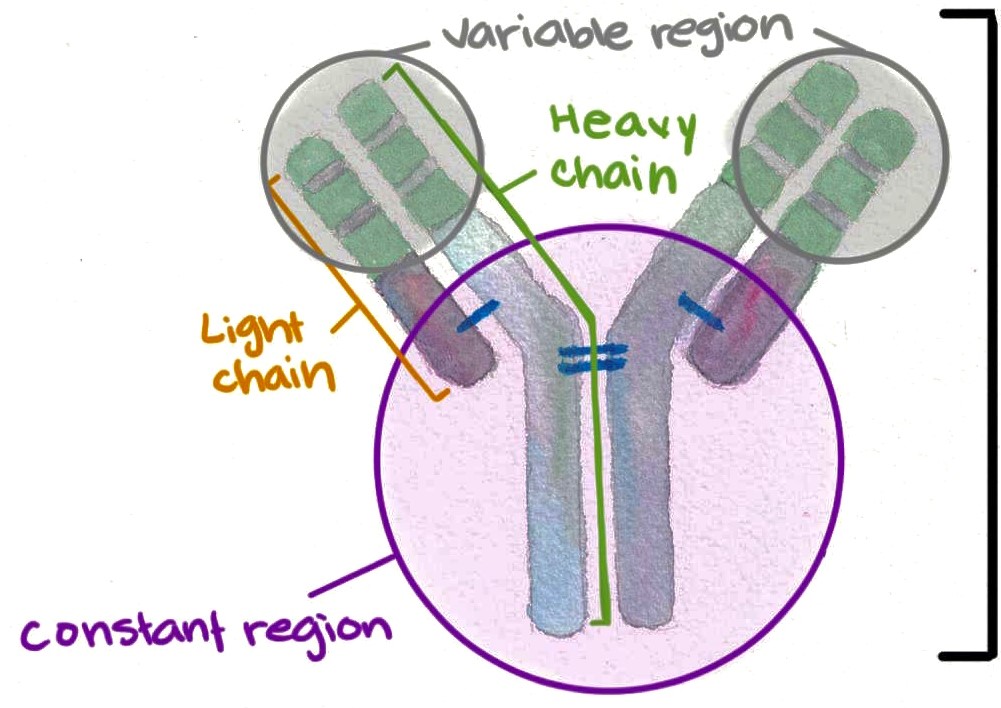
Structure of Immunoglobulins
Immunoglobulins consist of 4 peptide chains: 2 identical heavy chains (55KDa each) and two identical light chains (25 kDa each). This structure results in immunoglobulins having a 'Y' shape.
Heavy chains: Each heavy chain is made up of 420-440 amino acids. the two heavy chains are held together by disulfide bonds. A heavy chain is bound to a light chain through disulfide bond and other weak bonds including hydrogen bonds, hydrophobic bonds and salt linkages.
Light chains: Immunoglobulins have two light chains. Each light chain consists of 220-240 amino acids. Light chains can either be kappa or Lambda, and each immunoglobulin will either have two kappa or two lambda light chains, and never both types.
Variable regions: The amino terminal of the light and heavy chains consists of a region of variable amino acid sequence called the variable region. The variable region on the heavy chain is termed VH and VL for the corresponding region on the light chain. The variable region consists of three highly variable regions called hypervariable regions. The antigen binding site of the antibody molecule consists of 5-10 amino acids on both the heavy and light chains. These hypervariable regions confer the high specificity of the antibodies to various antigens.
Constant region: The carboxyl ends of both heavy and light chains consist of the constant region labeled CL and CH. The constant region of the heavy chain is responsible for the activation of the complement system, while the CL has no known biological function.
There are 5 types of immunoglobulins i.e., IgG, IgM, IgA, IgE and IgD.
Immunoglobulin G (IgG)
IgG has a molecular weight of 150,000 Da and a half-life of 23 days, which is the longest among all the immunoglobulins. It is the most abundant class of immunoglobulins making up about 80% of total serum Ig's. There are 4 subclasses of IgG's as follows.
- IgG1, IgG3 and IgG4 are able to cross the placenta so they play a significant role in protecting the developing fetus against infections.
- IgG1, IgG2 and IgG3 are effective in the activation of the complement system.
Immunoglobulin M (IgM)
IgM makes up about 5-8% of the serum Ig's and is present mostly intravascularly. its size is between 900,000 and 1,000,000 and has a half life of 5 days. IgM is a pentamer, consisting of 5 subunits. See figure below. This nature makes IgM have a higher valency to bind more antigens than the other Ig classes.
Immunoglobulin A (IgA)
IgA makes up 10 - 15% of serum Ig's. Serum IgA is present as a monomeric molecule with a molecular weight of 60,000 Da. It has a half life of 6-8 days. Secretory IgA is a dimer or tetramer and has a molecular weight of 70,000 Da. it is produced by epithelial cells of mucous membranes.
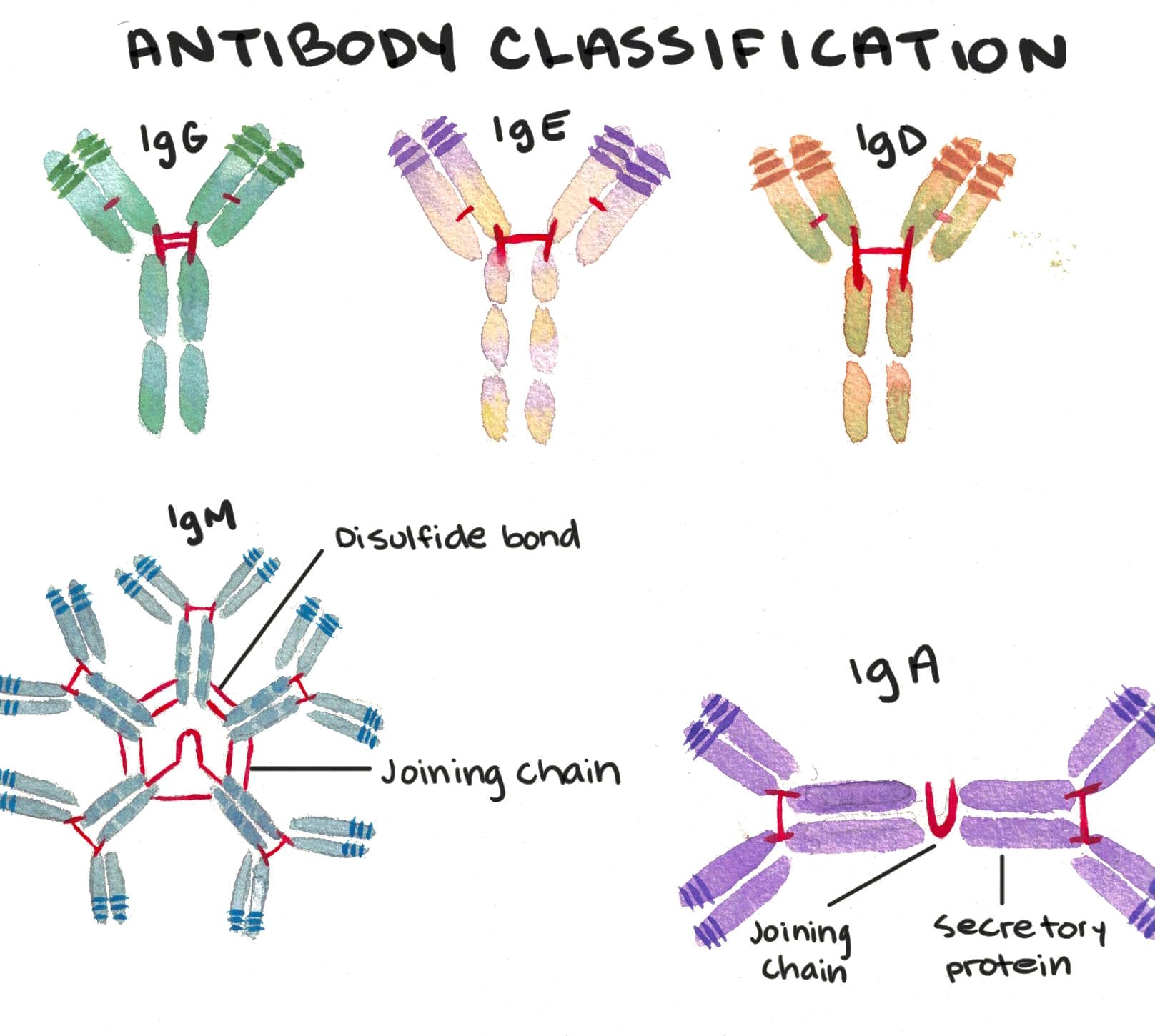
Immunoglobulin E (IgE)
Makes uo only 1% of Ig's. It is mostly found in lining of the respiratory and intestinal tracts. IgE has a molecular weight of 190,000 Da and a half-life of 2-3 days. IgE is responsible for the symptoms of hay fever, asthma, and anaphylactic shock. IgE induces basophils and mast cells to translocate their granules to the plasma membrane and release their contents to the extracellular environment in a process called degranulation. As a result, varieties of pharmacologically active mediators, such as histamine, are released and give rise to the symptoms associated with an allergic reaction.
Immunoglobulin D
Makes up less than 1% of total Ig's. It has a molecular weight of 180,000 Da and a half life of 2-3 days. Its function in the serum is yet to be elucidated.
Functions of Antibodies
- Neutralization: Antibodies bind onto antigens and prevent the antigens from binding to their targets, thereby preventing reducing disease progression. For example, antibodies would prevent a toxin from binding to its target tissues or could prevent a pathogen binding to its target cell.
- Opsonization: Antibody binding could opsonize the material and make it easy to be destroyed by macrophages or other phagocytic cells.
- Antibodies can cause activation of the complement cascade resulting in lysis of bacteria
Antigen Antibody Reactions
The interaction between antigens and antibodies is known as antigen–antibody reaction. These reactions are highly specific, and an antigen reacts only with antibodies produced by itself or by closely related antigens. These reactions are non-covalent bonds similar to the reactions between an enzyme and a sustrate, or signaling proteins binding to receptors. Antigen-antibody reactions are also reversible and can be inhibited by certain chemicals or physiological conditions.
Affinity refers to the intensity of attraction between an antigen and and an antibody. Low-affinity antibodies bind antigen weakly and tend to dissociate readily, whereas high-affinity antibodies bind antigen more tightly and remain bound for longer periods.
Avidity refers to the overall strength of binding an antigen with many antigenic determinants and multivalent antibodies. Avidity is a better measure of the strength of interactions in real biological systems than affinity.
Specificity denotes the ability of an individual antibody binding site to react with only one antigenic determinant.
Cross reactivity occurs when an antibody elicited by one antigen reacts with an unrelated antigen.
Antigen-antibody reactions occur in two stages: primary and secondary. Primary interaction is the initial interaction between antigen and antibody. It is rapid and reversible, but without any visible effects. Secondary stage is an irreversible interaction between antigen and antibody, with visible effects, such as agglutination, precipitation, neutralization, complement fixation, and immobilization of motile organisms. The binding between antigen and antibody during this stage occurs by covalent binding.
Humoral Immunity
There are two locations where a pathogen can reside in the animal's body: extracellularly in the tissue space, or intracellularly within the cell of the host. The body has two major processes to deal with these pathogens, Humoral immunity deals with extracellular pathogens and Cell Mediated Immunity deals with intracellular pathogens.
Humoral Immunity
The humoral response is mediated by antibodies. The production of antibodies follows a pattern:
- Lag phase occurs immediately following exposure to antigens. No antibodies are detected in circulation.
- Log phase is observed as a steady rise in antibody titers in circulation.
- Plateau phase is observed as an equilibrium phase where there is no significant change in antibody titers in circulation over time.
- Decline phase shows reduction in antibody titers. There is higher antibody catabolism than production.
Humoral response can be classified into two types:
Primary Response
When an individual is exposed to an antigen, for the first time, antibody response to the antigen takes a longer period (longer lag phase). The serum antibody levels increase for a long time (extended log phase) and then drops to very low levels. The lag phase is about 7-10 days or even longer (weeks) in some diseases. IgM is the first antibody to be produced, followed by IgG then IgA. IgM levels decline earlier than the other two.
Secondary Response
A secondary response occurs when an individual is exposed to an antigen (or a similar cross-reacting antigen) for the second time. During a secondary response, the lag phase is much shorter (3-5 days) and achieves higher antibody levels during the log phase. It has been shown that antibodies produced during a secondary response bind antigen more firmly.
Production of Antibodies
Antibodies are produced by plasma cells (which are activated B cells). Several theories have been proposed in the antibody production process including Instructive theory and Selective theory.
Factors affecting antibody production
Genetic factors: Individuals able to respond to an antigen are called responders, and those that do not are called non-responders. An immune response gene located on chromosome 6 also controls the immune response an individual can trigger.
Age: Age is a bigger factor when dealing with infants, as compared to adults. At birth, children are not fully immunologically competent. Immunological competence is achieved around 7 years.
Nutritional status: Deficiencies of certain amino acids and vitamins has been shown to reduce antibody production.
Route of exposure to antigen: Parenteral administration of the antigen induces a better immune response than oral or nasal routes.
Antigen dose: There is a minimal amount of antigen required to trigger an immune response. A very high dose of antigen might not trigger an immune response, a phenomenon called Immunological paralysis.
Multiple antigens: The response to multiple antigens is theoretically unpredictable (unless it has already been researched). The antigens might result in a greater combined immune response, or one antigen might hinder the immune response for the other antigen.
Adjuvants: These are substances that enhance the immunogenicity of an antigen.
Presence (or absence) of immunosuppressors: substances such as corticosteroids, radiation and some other drugs can suppress immunity. They are beneficial in cases of organ transplant, to inhibit the body from triggering an immune response to the organ. But they can also increase the individual's vulnerability/susceptibility to pathogens.
Cell Mediated Immunity (CMI)
CMI performs the following functions
It responds and confers immunity to diseases caused by intracellular pathogens. These include Mycobacterium tuberculosis, Brucella etc., viruses, intracellular fungi such as Histoplasma capsulatum, Blastomyces dermatitidis and intracellular parasites such as Toxoplasma gondii, Leishmania donovani etc.
Participates in immunity against cancer
It plays a role in development of delayed hypersensitivity reactions and some autoimmune diseases such as autoimmune thyroiditis.
Induction of Cell-Mediated Immunity
The induction of CMI follows the following steps:
- Presentation of foreign antigen to T lymphocytes by APCs.
- T cells recognizing the antigen
- Release of cytokines by Tc cells
Cytokines
Cytokines are substances secreted mainly by monocytes and lymphocytes and play significant roles in innate immunity, adoptive immunity and inflammation.
Main functions of cytokines
| Cytokine | Source | Function |
|---|---|---|
| Interleukin-1 (IL-1) | Macrophages | Activates helper T cells, causes fever |
| Interleukin-2 (IL-2) | Th-1 cells | Activates B cells, cytotoxic T cells and helper T cells. |
| Interleukin-3 (IL-3) | Th cells, natural Killer (NK) cells and Mast cells | Stimulates release of histamine |
| Interleukin-4 (IL-4) | Th-2 cells | Increases isotype switching and IgE, up-regulates expression of MHC class II. |
| Interleukin-5 (IL-5) | Th-2 cells | Stimulates B cell differentiation, increases eosinophils and IgA. |
| Interferon-α | Leukocytes | Inhibits replication of viruses |
| Interferon-β | Fibroblasts | Inhibits replication of viruses |
| Interferon-γ | Th-1, Tc and NK cells | Inhibits replication of viruses and stimulates phagocytosis by macrophages and NK cells. |
| Tumor necrosis factor (TNF) | Macrophages | Causes necrosis of tumors, activates neutrophils. Also has antiparasitic effects. |
| Transforming growth factor-β | Mast cells, Platelets and Lymphocytes | Causes increased IL-1 production, limits inflammation and promotes wound healing. |
Lymphoid Organs and Tissues
The immune response is mediated by the lymphoreticular system, which is a complex organization of cells and tissues distributed in different organs and tissues in the body.
Lymphoid organs are scattered throughout the body including gut associated lymphoid tissues such as tonsils, Peyer's patches and the appendix, and several other lymphoid tissue aggregates in the respiratory and genital and urinary tract.
The lymphoid tissues can be classified into Primary (Central) or Secondary (Peripheral) depending on their functions. Primary/Central lymphoid organs are the major sites for the synthesis of lymphoid cells. These organs can produce cells that act ac progenitors for other lymphoid cells. Primary lymphoid organs include the thymus and bone marrow. After the lymphoid cells mature, they are transferred to the peripheral organs, which include Lymph nodes, Spleen and other mucosa associated lymph aggregates.
The Thymus
The thymus is the first lymphoid organ to develop, it achieves maximum size at puberty and then atrophies. It consists of two major parts - the Cortex and the Medulla.
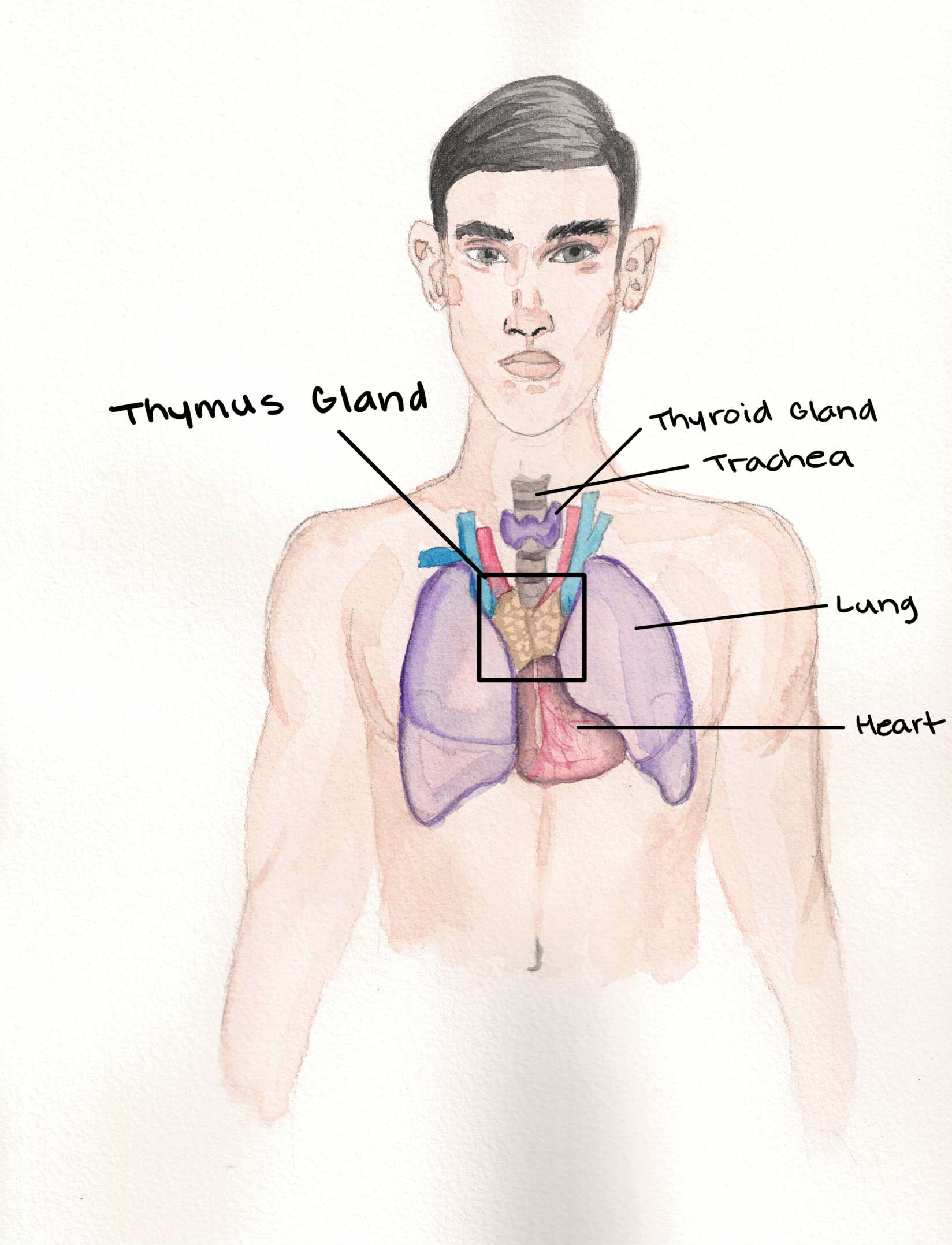
Image Source: National Cancer Institute - No changes made.
The Cortex: Consists of immunological immature T lymphocytes (named T due to their thymus origin) and a few macrophages and plasma cells.
The Medulla: Contains mature T lymphocytes. The concentric rings of squamous epithelial cells known as Hassall's corpuscles are found in the medulla.
Many types of T-lymphocytes are produced in the thymus to be able to respond to several antigens. The thymus results in the lysis of T cells that have reacted with self antigen, which would have resulted in autoimmunity.
The Bone Marrow
The lymphoid cells that develop in the bone marrow are called B cells named B due to their bone marrow (and Bursa of Fabricius in birds) origin. Immature B cells develop and differentiate in the bone marrow. This process is supported by stromal cells that produce various cytokines that are required for the development of the B cells. A process in the bone marrow selects the B cells that would malfunction (such as trigger autoimmunity) and destroy them. B cells are involved in antibody mediated immunity as they can secrete antibodies.
Lymph Nodes
Lymph nodes are spread out all over the body and range from 1 to 25 mm in diameter. They also have a cortex and a medulla. The cortex is densely populated with lymphocytes packed in follicles or nodules. The medulla is less densely populated with lymphocytes, it contains medullary cords which are long branching bands of lymphocytes and macrophages.
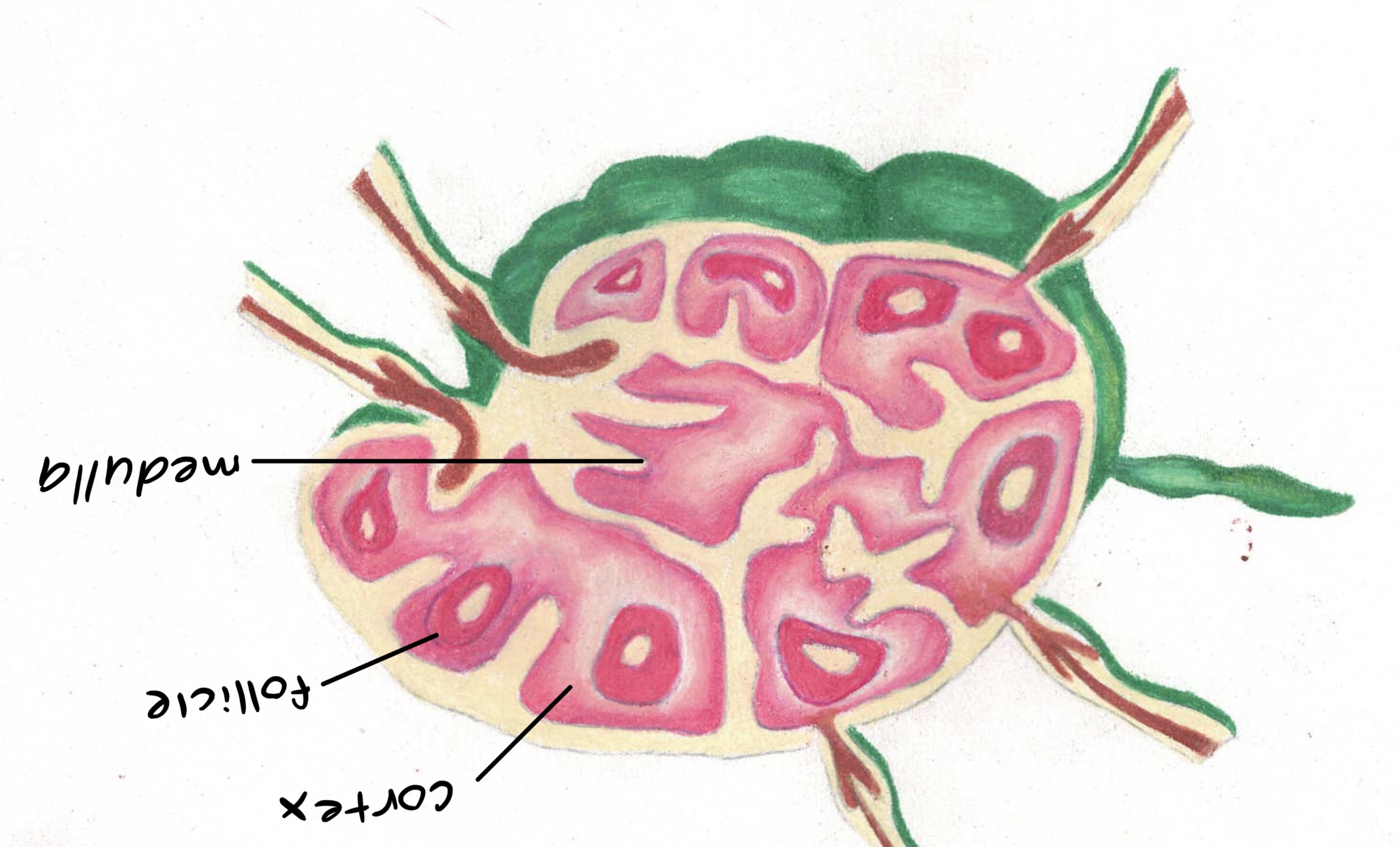
The structure of a lymph node.
The Spleen
The spleen is the largest lymphoid organ. its is ovoid in shape and located in the higher section of the left abdominal cavity. It is not supplied by the lymphatic system, like lymph nodes, instead, it is supplied by the splenic artery that brings in blood borne antigens and lymphocytes. as such, the spleen is important in preventing sepsis, which occurs more often in people who have undergone splenectomy.
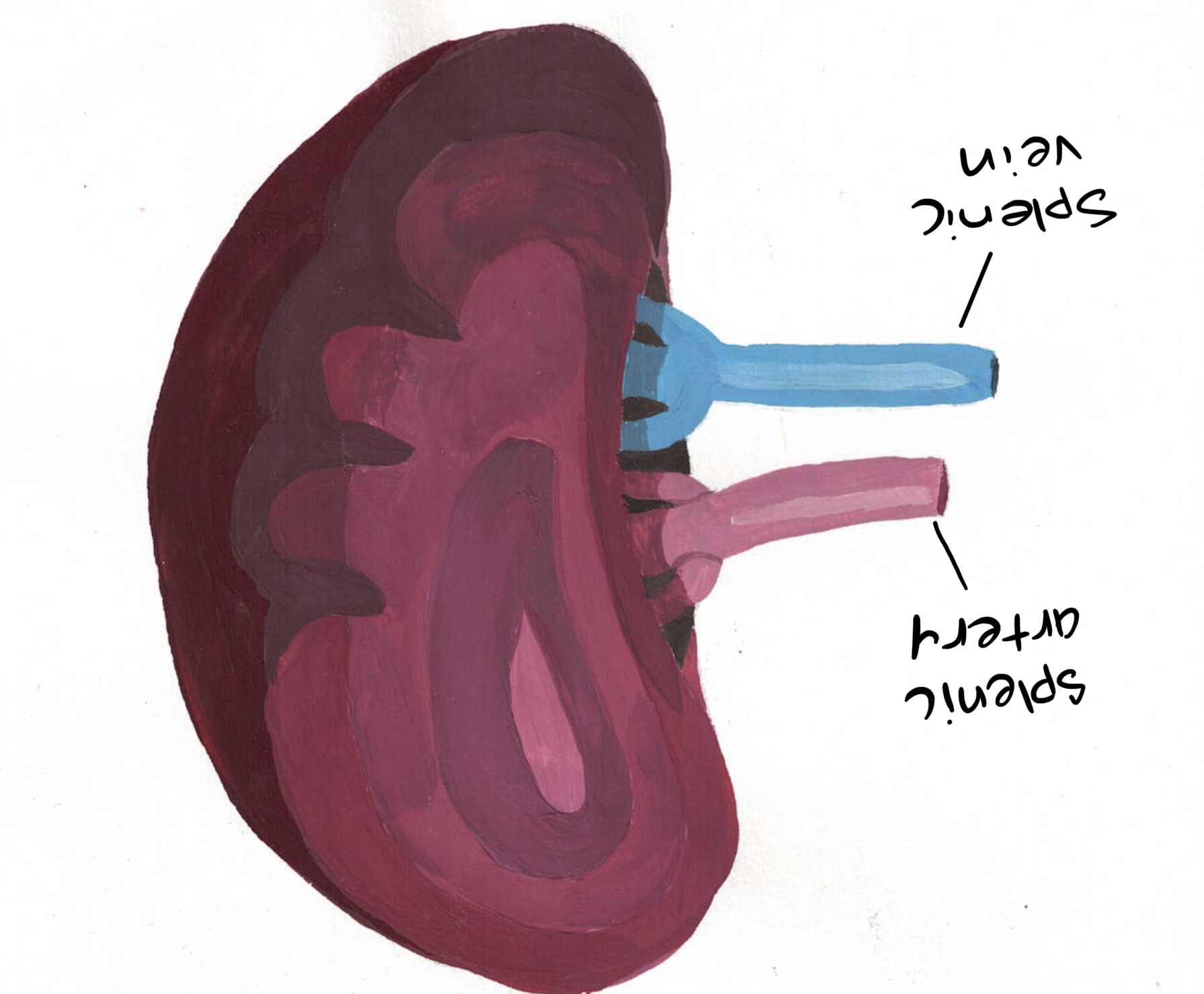
The morphology of the spleen.
Tonsils
These are located in the oropharynx and have a dense presence of B-lymphocytes. The oropharynx has a high level of antigenic stimulation to the exposure to the outside environment through the nose and mouth and the tonsils show evidence of active repetitive immune responses.
Peyer's patches
These are found located in the mucosal membranes of the intestines. The B cells differentiate into plasma cells and produce Immunoglobulin A (IgA). Some specialized epithelial cells called M cells deliver bacteria and viruses to macrophages then the engulfed material is presented to T and B lymphocytes.
Types of Immune Cells
Lymphocytes
The lymphocytes are the most important of the leukocytes due to their ability to interact with antigenic substances, to react with non-self antigens and their role in the development of memory in the immune system.
The lymphocytes themselves are diverse, varying in their lifespan, function, surface structure etc. Lymphocytes are classified into T lymphocytes / T cells, B lymphocytes (B cells).
T Cells
T cells are derived from the thymus. They play an important role in adaptive immunity
T cells make up about 65-80% of the small lymphocytes in blood. They have a long lifespan ranging from months to years. T lymphocytes perform two main functions:
- Regulation of immune response: This is achieved primarily by helper (CD4+) T cells, which produce interleukins. (CD4+) T cells make up 655 of all T cells. The CD4 displayed on the surface of these cells recognize a non-peptide binding portion of MHC class II molecules. They help B cells to be transformed into plasma cells. They help (CD8+) T cells to become active cytotoxic T cells. and they help macrophages to mediate delayed hypersensitivity reactions.
- Effector functions: These are mediated by CD8+ T cells, which are also called cytotoxic T (Tc) cells and suppressor T (Ts) cells. They are found mainly in the bone marrow and gut lymphoid tissue. CD8+ T cells perform cytotoxic functions killing virus-infected cells, allograft cells and tumor cells.
There are two signals that are important for the activation of T cells: The interaction of the antigen and the MHC protein with the T cell-receptor-specific antigen. Secretion of interleukin 1 (IL-1) secreted by the macrophages is also necessary for helper T-cell activation. Secondly, a B7 protein on the antigen presenting cell (APC) must interact with CD28 protein. This results in the production of Interleukin 2 (IL-2) which is essential in producing T helper cells capable of regulatory, effector and memory functions.
Memory T cells
Memory T cells are responsible for initiating a rapid and vigorous immune response for many years after an initial exposure to an antigen or microbe. A large number of memory cells are produced, which makes the secondary response greater than the primary response.
Superantigens
Unlike regular antigens, which stimulate one or just a few helper cells, superantigens stimulate a large number of helper T cells. An example of a superantigen is the staphylococcal toxic shock syndrome. In this case, a toxin produced by S. aureus binds directly to class II MHC proteins without internal processing, resulting in activation of T cells and release of interleukin 2 and tumor necrosis factor (from macrophages). These are responsible for the clinical signs observed in this disease (sudden high fever, increased blood pressure, skin rash and vomiting/diarrhea.
B cells
B cells and named because in birds, they differentiate in the bursa or Fabricius located in the caudal end of the gut. There is yet no evidence of the presence of an organ similar to the bursa of Fabricius in other animals. Activation of B cells involves a complex interaction of IL-4, IL-5 (produced by the helper T cells, CD28 (T cells) and B7 protein (B cells). These interactions are also important in determining which Immunoglobulin will be secreted. For example, the CD40L-CD40 interaction is needed for the switch from IgM to IgG to take place.
Activation of B cells results in the production of many plasma cells that produce large amounts of antibodies/immunoglobulins specific for the antigen epitope. Some activated B cells produce memory cells that contain IgG or IgM. These get reactivated rapidly during re-exposure to the same antigen.
Antigen-presenting cells (APCs)
APCs include macrophages and dendritic cells.
Macrophages
The mononuclear phagocytic cells are composed of monocytes (in blood) and macrophages (in tissues). Monocytes are considered as macrophages in transit, and they become true macrophages when they embed inside the tissues. Monocytes, together with other granulocytes have phagocytic activity, i.e. can engulf particulate matter including microbes, cells and inert particles. Macrophages are 5-10 times larger than monocytes and generally have increased organelles, have higher phagocytic activity and produce higher levels of hydrolytic enzymes. Different organs and tissues have macrophage-like cells named according to the organ where they are located. The lungs have alveolar macrophages, liver (Kupffer cells), kidneys (mesangial cells) brain (microglial cells), bones (osteoclasts) and connective tissues (histiocytes). Macrophages can be activated by several cytokines, some components of the bacterial cell wall and some inflammatory mediators.
Macrophages perform three main functions: phagocytosis (most important function), antigen presentation and cytokine production.
Dendritic cells
Dendritic cells possess long, narrow processes that make them resemble neurones. These processes make these cells very efficient at making contact with foreign materials. They are most commonly present in the skin (where they called Langerhans cells) and the mucosa. They can migrate to lymph nodes to present the antigens to helper T cells. There are 4 types of dendritic cells: Langerhans cells, Myeloid cells, Lymphoid dendritic cells and interstitial dendritic cells.
Plasma cells
Plasma cells result from the maturation (differentiation) of B cells. Plasma cells produce all classes of Immunoglobulins. They are found in the bone marrow and only have a short lifespan of about 30 days.
Natural killer cells
NK cells are larger granular lymphocytes. They are called NK cells because they can kill cells infected with certain viruses and tumor cells. They develop in the bone marrow and possess receptors called killer activation and killer inhibition receptors. They kill those cells by secreting cytotoxins such as perforins.
Granulocytes
Granulocytes are classified as Neutrophils, Eosinophils and Basophils based on shape and staining properties. Neutrophils and eosinophils are phagocytic but basophils aren't. Mast cells are also granulocytes located in various organs in the body including the skin, mucosa of respiratory, genital and urinary tract, digestive system etc. They contain granules that contain histamine. Histamine is an important substance in the development of allergies.
The Major Histocompatibility Complex (MHC)
The major histocompatibility complex (MHC) is a large locus on vertebrate DNA containing a set of closely linked polymorphic genes that code for cell surface proteins essential for the adaptive immune system. These cell surface proteins are called MHC molecules. In a cell, protein molecules of the host's own phenotype or of other biologic entities are continually synthesized and degraded. Each MHC molecule on the cell surface displays a small peptide (a molecular fraction of a protein) called an epitope. The presented self-antigens prevent an organism's immune system from targeting its own cells. The presentation of pathogen-derived proteins results in the elimination of the infected cell by the immune system.
MHC class I
MHC class I molecules are expressed in all nucleated cells and also in platelets. It presents epitopes to killer T cells, thus, MHC class I helps mediate cellular immunity, a primary means to address intracellular pathogens, such as viruses and some bacteria
MHC class II
MHC class II occurs only on antigen-presenting cells (APCs): macrophages, B cells, and dendritic cells (DCs). An APC takes up an antigen, processes it, and returns a fraction of it (an epitope) and displays it on the APC's surface coupled within an MHC class II molecule (This, in essence, is the process of antigen presentation).
MHC class III
Class III molecules secrete components of the complement system (such as C2, C4, and B factor), cytokines (such as TNF-α, LTA, and LTB), and heat shock proteins.
Immunological Tolerance
Immunological tolerance is a state of specific immunologic unresponsiveness to an antigen that a person has had prior exposure to. Some of the possible mechanisms include.
- Clonal Deletion
- Clonal Anergy
- Suppression
Immune tolerance could be Natural tolerance - develops during embryonic development, or Acquired tolerance- occurs when an immunogen induces unresponsiveness to itself.
Immunodeficiency
Immunodeficiency, also known as immunocompromisation, is a state in which the immune system's ability to fight infectious diseases and cancer is compromised or entirely absent. In most cases, immunodeficiency is acquired (secondary) due to extrinsic factors such as HIV infection and environmental factors, such as nutrition. Immunosuppression as a result of some drugs, such as steroids, can either be an adverse effect or the intended purpose of the treatment.
Types of Immunodeficiency (by Cause)
- Humoral immune deficiency (include B cell deficiency or dysfunction). Characterised by repeated mild respiratory infections. In extreme cases, agammaglobulinemia, which is lack of all or most antibody production, results in more frequent severe infections and is often fatal.
- T cell deficiency often causes secondary disorders such as acquired immune deficiency syndrome (AIDS).
- Granulocyte deficiency, including decreased numbers of granulocytes (called as granulocytopenia or, if totally absent, agranulocytosis). If affecting neutrophils, it's termed neutropenia.
- Asplenia, where there is no function of the spleen.
- Complement deficiency is where the function of the complement system is deficient.
In most individuals, immunodeficiency will be caused by multiple factors.
Hypersensitivity
Hypersensitivity (also called intolerance) refers to an immune response charecterized by exaggerated or inappropriate reactions that are harmful to host. It is a harmful immune response in which tissue damage is induced by exaggerated or inappropriate immune responses. It may occur in an individual who is sensitized or on re-exposure to the same antigen.
Hypersensitivity reactions can be classified into four types.
- Type I - IgE mediated immediate reaction
- Type II- Antibody-mediated cytotoxic reaction (IgG or IgM antibodies)
- Type III- Immune complex-mediated reaction
- Type IV- Cell-mediated, delayed hypersensitivity reaction
Type I hypersensitivity occurs as a result of exposure to an antigen. The response to the antigen occurs in two stages: the sensitization and the effect stage. In the 'sensitization' stage, the host interacts with the antigen but does not indicate any symptoms. Subsequently, in the "effect" period, the pre-sensitized host is re-introduced to the antigen, which then leads to a type I anaphylactic or atopic immune reaction.
Several types of antigens can cause a Type I reaction including,
- Foods such as nuts, eggs, soy, wheat, shellfish, etc.
- Animal source: bee, wasp, cats, insects, rats, etc.
- Environmental factors: dust mites, latex, pollen, mold, etc.
- Atopic diseases: allergic asthma, allergic rhinitis, conjunctivitis, dermatitis, etc.
- Medication-induced reactions: antibiotics
Type II hypersensitivity reaction denotes an antibody-mediated immune reaction in which antibodies (IgG or IgM) are directed against cellular or extracellular matrix antigens with the resultant cellular destruction, functional loss, or damage to tissues.
Type II hypersensitivity reactions can be broadly classified into three types:
Cell depletion or destruction without inflammation
Inflammation mediated by complement or Fc receptor
Cellular dysfunction by antibodies
The process involves a series of immune-mediated events that might take different forms.
Type III hypersensitivity reaction, an abnormal immune response is mediated by the formation of antigen-antibody aggregates called "immune complexes." They can precipitate in various tissues such as skin, joints, vessels, or glomeruli, and trigger the classical complement pathway. Complement activation leads to the recruitment of inflammatory cells (monocytes and neutrophils) that release lysosomal enzymes and free radicals at the site of immune complexes, causing tissue damage. The most common diseases involving a type III hypersensitivity reaction are serum sickness, post-streptococcal glomerulonephritis, systemic lupus erythematosus, farmers' lung (hypersensitivity pneumonitis), and rheumatoid arthritis.
Type IV hypersensitivity reactions are, to some extent, normal physiological events that help fight infections, and dysfunction in this system can predispose to multiple opportunistic infections. Adverse events can also occur due to these reactions when an undesirable interaction between the immune system and an allergen happens.
Anaphylaxis
Anaphylaxis is an acute, potentially fatal, and systemic manifestation of immediate hypersensitivity reaction. It occurs when an antigen (allergen) binds to IgE on the surface of mast cells with the consequent release of several mediators of anaphylaxis.
The effector cells in anaphylaxis include (a) mast cells, (b) basophils, and (c) eosinophils. All these three cells contain cytoplasmic granules whose contents are the major mediators of allergic reactions.
Many substances instead of a single substance are responsible for all manifestations of anaphylaxis. Important mediators include (a) histamine, (b) slow-reacting substances of anaphylaxis (SRS-A), (c) serotonin, (d) eosinophilic chemotactic factors of anaphylaxis, and (e) prostaglandins and thromboxanes.
Histamine is the most important mediator of anaphylaxis. It is found in a preformed state in granules of mast cells and basophils. It causes vasodilatation, increased capillary permeability, and smooth muscle contraction. It is the principal mediator of allergic rhinitis (hay fever), urticaria, and angioedema. Antihistamines that block histamine receptors are relatively effective against allergic rhinitis but not against asthma.
Clinical manifestations of anaphylaxis
Anaphylaxis is an acute, life-threatening reaction usually affecting multiple organs. The time of onset of symptoms depends on the level of hypersensitivity and the amount, diffusibility, and site of exposure to the antigen. Multiple organ systems are usually affected, including the skin (pruritus, flushing, urticaria, and angioedema), respiratory tract (bronchospasm and laryngeal edema), and cardiovascular system (hypotension and cardiac arrhythmias). When death occurs, it is usually due to laryngeal edema, intractable bronchospasm, hypotensive shock, or cardiac arrhythmias developing within the first 2 hours
Prevention and Management of anaphylaxis
Acute desensitization involves the administration of small amounts of antigen to which the person is sensitive, at an interval of 15 minutes. The antigen is introduced in small quantities; hence enough mediators are not released to result in a major reaction.
Chronic desensitization involves the long-term administration of antigen to which the person is sensitive, at an interval of weeks. This stimulates the production of IgA- and IgG-blocking antibodies that prevent subsequent antigen to binding to mast cells, therefore, preventing the reaction.
Autoimmunity
Autoimmunity is a condition when the body produces autoantibodies and immunologically competent T lymphocytes against its own tissues. Conditions where the mechanisms of self-tolerance fail are termed as autoimmune disorders and the phenomenon is called autoimmunity
Certain individuals are genetically susceptible to developing autoimmune diseases. This susceptibility is associated with multiple genes plus other risk factors. Genetically predisposed individuals do not always develop autoimmune diseases. Three main sets of genes are suspected in many autoimmune diseases. These genes are related to:
- Immunoglobulins
- T-cell receptors
- The major histocompatibility complexes (MHC).
Organ specific autoimmune diseases arise when autoantibodies are produced targeting only the tissue of a single organ, thus affecting that organ solely. A few examples of such disorders are Addison's disease, autoimmune hemolytic anemia, Goodpasture's syndrome, Graves' disease, Hashimoto's thyroiditis, idiopathic thrombocytopenic purpura, insulin-dependent diabetes mellitus, myasthenia gravis, pernicious anemia, poststreptococcal glomerulonephritis, etc.
Systemic Autoimmune Diseases arise when autoantibodies are produced against a wide range of host tissues in systemic autoimmune diseases. These diseases reflect a general defect in immune regulation that results in hyperactive T cells and B cells. Tissue damage is widespread, much more generalized and usually leads to multisystem disorders. Tissue damage is caused by cell-mediated immune responses, by autoantibodies, or by the accumulation of immune complexes. An example of a systemic autoimmune disease include Systemic lupus erythematosus (SLE). SLE (Lupus) is an autoimmune disease in which the body's immune system mistakenly attacks healthy tissue in many parts of the body. Symptoms vary between people and may be mild to severe. Common symptoms include painful and swollen joints, fever, chest pain, hair loss, mouth ulcers, swollen lymph nodes, feeling tired, and a red rash which is most commonly on the face. Often there are periods of illness, called flares, and periods of remission during which there are few symptoms.
Transplant Immunology
Transplantation is the transfer of cells, tissues, or organs from one site in an individual to another, or from one individual (the donor) to another (the recipient).
Types of transplants include:
- Autograft: An autograft is the transfer of individual's own tissue or organ from one site to another site in the body. In other words, the recipient is also the donor. Examples of autografts include skin transplants in burn patients and bypass surgery in patients suffering from coronary heart disease.
- Syngraft: A syngraft is a transfer of tissue between two genetically identical individuals.
- Allograft: An allograft is the transfer of tissue or an organ between genetically different members of the same species, i.e., from one human to another. This is the most common form of transplantation.
- Xenograft: A xenograft is the transfer of tissues or organs between members of different species. It is always rejected by an immunocompetent recipient.
Tumor Immunology
Tumors or neoplasias develop when the balance between cell death and renewal is disturbed in a way that numerous clones of a single cell group are produced in an uncontrolled fashion. Tumor immunology deals with the antigens on tumor cells and the immune respose to these antigens. Tumor cells may express developmental antigens that are usually seen observed in the prenatal period e.g., alpha-fetoprotein and carcinoembryonic antigen.
Cancer antigens are capable of eliciting a comprehensive immune response involving both the cellular and humoral immune responses. T lymphocytes play an important role in tumor immunity acting both as cytotoxic effector cells and as central modulating cells. Through these effector cells, they control the specific cell mediated antitumor immune responses and upregulate non specific killing mechanisms. B lymphocytes produce tumor-specific antibodies, which may induce complement-dependent cytotoxicity of tumor cells.