Course Detail
Microbiology
Microbiology is the study of microorganisms including bacteria, viruses, fungi, and some parasites. Most of these organisms are studied within the concept of causing diseases in humans, animals, and plants. Broadly, microbiology also includes the study of microbial pathogenesis, disease pathology, immunology, and epidemiology of the resultant diseases.
List of Contents
- History of Microbiology
- Microscopy and Staining
- Morphology and Physiology of Bacteria
- Sterilization and Disinfection
- Bacterial Cultures
- Bacterial Taxonomy
- Bacterial Taxonomy
- Microbial Genetics
- Microbial Biotechnology
- Microbial Pathogenicity
- Antimicrobial Compounds
History of Microbiology
Microbes are the most significant biological forms in the planet interacting with humans because of their pervasive presence. Microbes may have either beneficial role in maintaining life or undesirable consequences causing disease in humans, animals and plants. Diseases caused by microbes vary in severity from mild infections to severe diseases such as tuberculosis.
Microbial diseases have shaped global history for many ways. In 1347, Bubonic plague or Black Death started to spread in Europe and about 4 years later, (1351) the plague had killed one-third of the population (an estimate of 25 million people). Over the next 80 years, the disease remerged frequently and had killed about 75% of the European population.
Another example started towards the end of 2019. A viral disease (later named Covid-19) caused by a coronavirus strain started to ravage the global population causing millions of deaths across the globe. At the time of this article, there has been 3.3 million deaths globally.
These are just examples from many such epidemics and pandemics, which resulted in extensive deaths of people irrespective of economic and social stature. Other epidemics that have had significant consequences include smallpox, malaria, measles, and polio.
The first person to observe and describe microorganisms was Antony van Leeuwenhoek who spent most of his spare time tinkering with convex glasses to make simple microscopes. The microscopes could magnify organisms 50-300 times and he was able to observe both bacteria and protozoa.
Although microorganisms had been observed under the microscope, there was significant disagreement as to their origin. Spontaneous generation was one of the theories proposed. In this theory, microorganisms were believed to originate from non-living things.
Louis Pasteur is known by most as the father of Microbiology. He even coined the name 'micro'-'biology' as the study of microscopic organisms. He proposed the 'Germ theory of disease' after several experiments and proved that all life arose only from their like, thereby disproving the theory of spontaneous generation.

(Photograph originally posted by Albert Edelfelt)
Louis Pasteur also developed the pasteurization process, a process used to kill microbes in liquids by heating followed by rapid cooling. This technique is now commonly used in preservation of fruit juices and milk.
Louis also observed that some organisms required oxygen for their survival and growth, while others did not require oxygen. He called these aerobic and anaerobic microorganisms, respectively.
Louis Pasteur was the first to demonstrate the concept of vaccination. He attenuated the bacillus anthracis organisms by incubation at 42oC and then inoculated the attenuated bacteria into animals. He later observed that inoculated animals developed a certain level of protection against Anthrax. In 1885, Louis developed the Rabies vaccine.
Joseph Lister is known for his contributions in the development of antiseptics. He designed antiseptic surgery to prevent wound infection using heat sterilization.
The Koch's Postulates
(Photograph from Wilhelm Fechner - Public Domain.)
Robert Koch demonstrated that Anthrax was caused by a bacterium (Bacillus anthracis). His criteria for demonstrating a microorganism as the cause of a disease is published as the Koch's postulates, which include:
- The microorganism must be present in every case of the disease, and absent in every healthy case.
- The microorganism must be grown in a pure culture from samples obtained from diseased lesions.
- The pure culture of microorganism will cause a similar disease if injected into a suitable laboratory animal.
- The same organism must be isolated again in pure culture from lesions of the inoculated laboratory animals.
Solid Media for bacterial growth
Koch pioneered the use of agar as a base for culture media. This enabled the isolation of pure cultures that contained only one type of bacteria. Koch also developed meat based or protein-based culture media for isolating bacteria from the body. These media resembled the composition of body fluids and are used to develop nutrient broths or nutrient agar that are still in widespread use today.
Microscopy and Staining
A microscope is an instrument that uses one or multiple lenses to produce a magnified image of an object that would have been invisible to the naked eye.
There are three main types of microscopy techniques that will be covered in detail in this course.
Light Microscopy
As the name suggests, light microscopy uses natural or artificial light to illuminate the object for viewing. Light increases the resolving power of the microscope (Resolution is the ability of the microscope lens to distinguish two closely adjacent objects as distinct separate entities.) The resolving power of a light microscope can also be enhanced by changing the medium through which light passes. For example, the use of emersion oil helps to improve the resolution of the microscope. There are 4 types of light microscopy as described below:
1. Bright-Field Microscopy: Also called 'Ordinary light microscopy' being the most common type of light microscopy. It contains compound lens, containing multiple objective lens and a fixed ocular lens. The total magnification is the product of the magnifications of objective lens and ocular lens (such as X10 and X40 to make a total magnification of X400).
Dark-field microscopy: (also called Dark-ground microscopy. This makes use of a dark-ground microscope, which uses reflected light rather than
transmitted light. This prevents light from directly falling on the objective lens. The object appears brightly stained against a dark background.

An image as it appears under a dark field microscope. - Source Wikipedia. Under
Creative Commons Licence - Public Domain. No alterations.
Dark field microscopy is good for demonstrating flagellated bacteria and protozoa, or observing very thin bacteria such as spirochetes, not visible under
ordinary light microscopes.
Phase-contrast microscopy: Uses a specific optical system that converts differences in density in an organism into differences in light intensity
resulting in light and dark contrast within the image. It is useful for examining the internal structures of a living cell.
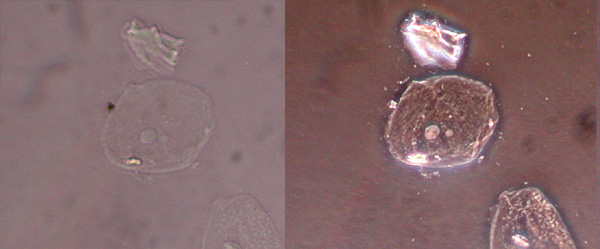 Left: Image under an ordinary microscopy. Right: Same image as it appeared under a phase-contrast
microscopy. Source Wikipedia. Under
Creative Commons Licence - Public Domain. No alterations.
Left: Image under an ordinary microscopy. Right: Same image as it appeared under a phase-contrast
microscopy. Source Wikipedia. Under
Creative Commons Licence - Public Domain. No alterations.
Interference microscopy: This is used for demonstrating cell organelles or quantitative measurement of the chemical constituents of the cells, such as proteins, lipids, and nucleic acids.
Fluorescence microscopy
Fluorescence microscopy uses fluorescent dyes to stain the object / specimen, and once viewed under UV light, the object appears as brightly glowing against a dark background.
Some examples of fluorescent dyes used to visualize bacteria include: Auramine O, acridine orange, and rhodamine.
Electron microscopy (EM)
Electron microscopy utilizes a beam of electrons (instead of light). The object is placed on the path of the electron beam causing the electrons to scatter and produce an image, which is displayed on a screen. Because electrons have a very low wavelength (0.005nm) as compared to the wavelength of visible light (5000 nm), electron microscopes can have a resolution about 100,000 times higher than light microscopes.
There are several techniques that have been developed for electron microscopy including:
- Shadow Casting: Is performed by depositing a thin layer of platinum on the microorganism. The image is displayed on a fluorescent screen.
- Scanning electron microscopy: Displays a 3D image of the object at a high resolution.
- Freeze-etching: Allows for objects to be observed when they are still alive. (Other EM techniques cannot visualize live cells).
- Immunoelectron microscopy: The specimen is reacted with specific antiviral antibody that results in clumping of viral particles.
Bacterial Microscopy
Bacteria can be visualized under a microscope in either stained or unstained (wet mount) preparations. Unstained preparations can be used to demonstrate motility, while stained preparations are best for demonstrating structural details due to the color contrast.
Staining Methods
1. Simple Stains: Such as Methylene Blue provide color contrast but cannot be used to differentiate different bacterial species on the same specimen.
2. Negative Staining: In this staining technique, the bacteria remain unstained, but their background is. Using stains such as Indian ink, the background becomes dark. It can be used to demonstrate bacterial capsules that usually cannot take stains when using simple staining techniques.
3. Impregnation Stains: This technique is used to observe cells or structures that are too thin. Silver impregnation is used to make such structures visible.
4. Gram Staining: Is a differentiation staining method used to identify Gram-positive and Gram-negative bacteria groups. This technique consists of four steps:
a. Primary Staining using a basic dye such as methyl violet
b. Addition of dilute iodine solution as a mordant
c. Decolorization using Ethanol, acetone, or aniline
d. Counterstaining with acidic dye such as carbol fuchsin, safranine or neutral red.
Gram-positive bacteria are those that resist decolorization and retain the primary dye-iodine complex, appearing violet. Gram-negative bacteria are decolorized by organic solvents and take the counterstain, appearing red.
There are some bacterial species such as Mycobacterium tuberculosis and Mycobacterium leprae that have a waxy envelope containing complex glycolipids that make them impervious to the Gram stain. Therefore, it is impossible to classify them as either Gram +ve or -ve.
Morphology and Physiology of Bacteria
Living things can be classified into three kingdoms: Plant, Animals and Protista. Microorganisms belong to the kingdom Protista. This kingdom consists of single celled organisms such as bacteria, fungi, algae and protozoa. The kingdom is further divided into three groups: Prokaryotes, Eukaryotes and Archaebacteria.
Bacteria are very small; their size is measured in microns (micrometer). 1 micron (µ) is equal to 1/1000 millimeters. Most bacteria of medical importance measure 2-5 microns in length.
Bacteria Shape
1. Cocci: Cocci are oval or spherical shaped cells. These may be arranged in pairs (such as, pneumococci), tetrads (such as, micrococci), chains (such as, streptococci), and clusters (such as, staphylococci).
2. Bacilli: Bacilli (singular bacillus) are rod shaped. Bacilli
occur in one of the following arrangements
(a) Coccobacilli: Length of the bacteria is approximately the same
as its width, for example, Brucella.
(b) Streptobacilli: These are arranged in chains, such as, Streptobacillus.
(c) Comma shaped: These occur in a curved shape, such as, Vibrio.
(d) Spirilla: These are rigid spiral shapes, such as, Spirillum.
3. Spirochetes: Spirochetes are slender, flexuous spiral shapes, such as, Treponema.
4. Actinomycetes: Actinomycetes are branching filamentous bacteria resembling the shape of fungi.
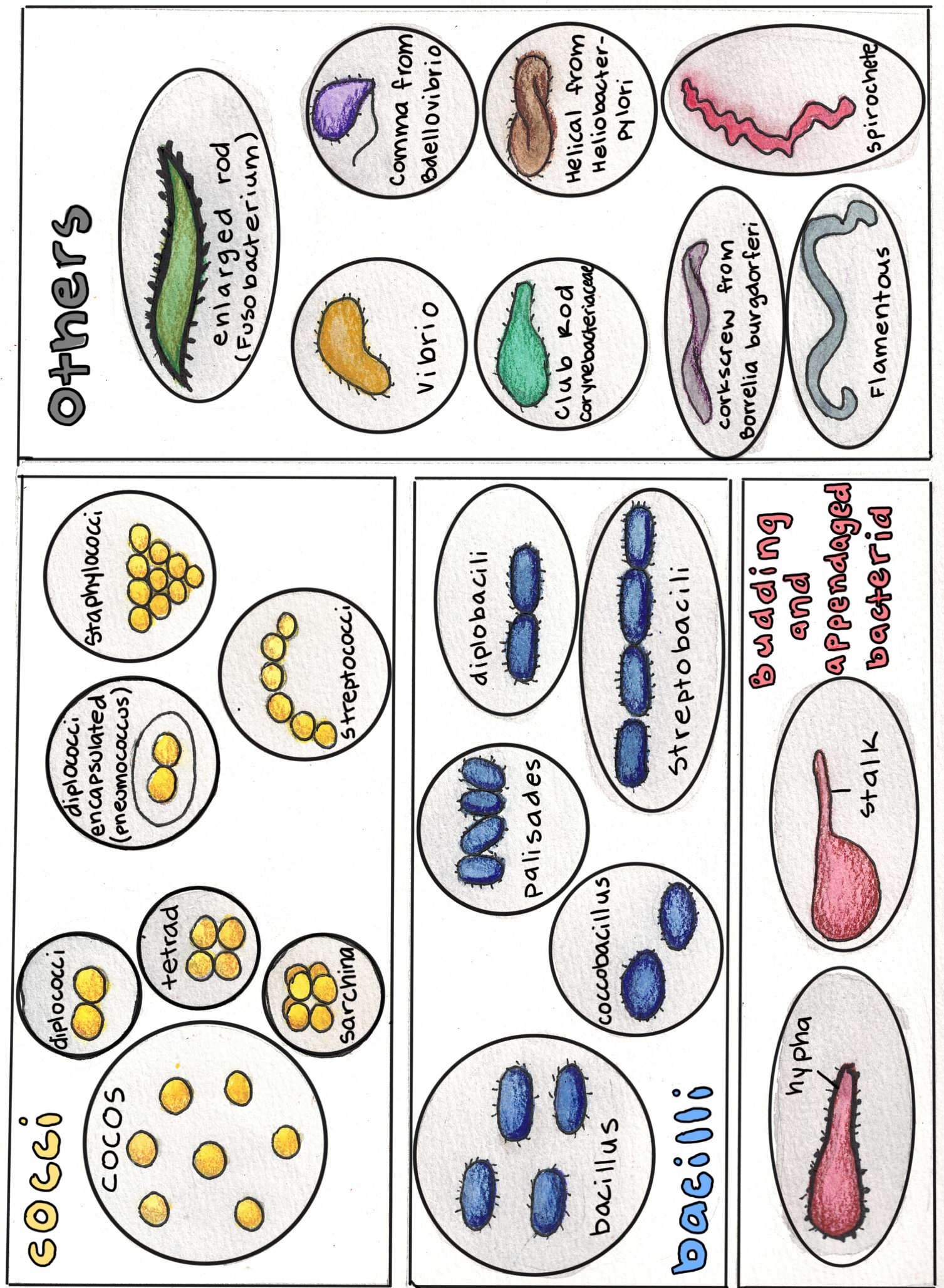
Image created by Tensai.org. All rights reserved.
Bacterial Cell Wall
Bacteria are bound by a rigid cell membrane and well wall. The cell wall is composed of peptidoglycan and is responsible for the shape of the cells. Peptidoglycan is a disaccharide with two sugar derivatives joined together by a peptide chain. The cell wall of gram +ve bacteria is thick and is made up of multiple layers of peptidoglycan. The gram-negative cell wall is more complex but contains less peptidoglycan at about 1-2 layers. The gram-negative cell wall also contains lipoprotein, outer membrane and lipopolysaccharides.
Bacterial Cell Membrane
The plasma membrane is thin and acts as an osmotic barrier. It lies underneath the cell wall. It contains phospholipids and proteins such as enzymes. However, unlike eukaryotic plasma membranes, the bacterial cell membrane does not contain cholesterol.
Ribosomes
Located within the cytoplasm, bacterial ribosomes are smaller (70S) than eukaryotic ribosomes (80S). They have two subunits (30S and 50S). They function in protein synthesis (translation).
Mesosomes
Mesosomes are convoluted vesicles formed as invagination of the plasma membrane into the cytoplasm. They are analogs of mitochondria in eukaryotes, and they perform similar functions related to energy metabolism.
Inclusion bodies
The main function of these vesicles is believed to be storage. Some vesicles store organic molecules such as glycogen while others store inorganic substances such as sulfur. Different types of granules can be detected by special staining techniques. Starch granules can be detected using iodine stains, while lipid granules can be demonstrated using Sudan black dye.
Bacterial Nucleus
Unlike eukaryotic cells, the bacterial nucleus is not bound by a nuclear membrane. There is also no nucleolus. The nucleus is basically the region where the DNA is located. Bacterial DNA is a circular double stranded structure measuring about 1000(µ) when stretched straight. The DNA is located in a region called the nucleoid, or sometimes referred to as the chromosome. Bacteria also contain extrachromosomal DNA called plasmids. Plasmids are circular double stranded DNA molecules that replicate independently. They are not required for growth but sometimes they carry genes that result in antibacterial resistance, or the ability for bacteria to produce toxins.
Capsule
The bacterial capsule is a gel-like layer formed on top of the cell wall. When its narrower, its called a microcapsule. The colloidal material secreted by some bacteria is called slime or glycocalyx. The bacterial capsule is made up of polysaccharides referred to as exopolysaccharides. In some species (such as Bacillus anthracis, the capsule is made up of poly-amino acids.
The capsule has several functions including:
- Preventing the host from initiating an immune response including phagocytosis.
- Enables the bacteria to adhere to mucosal membranes
- Plays a role in bacteria being able to resist drying and other harsh environmental conditions.
The capsule can be observed under the microscope using special staining methods such as the Welch method, which uses Copper as a mordant. The M'Fadyean capsule stain, which uses polychrome methylene blue stain, is used to observe the Bacillus anthracis capsule. Other methods used to observe the bacterial capsule include Negative staining with India ink and Other Serological staining methods.
Bacterial Flagella
These are thread-like appendages embedded in the cell envelope. These structures are responsible for motility and may a role in bacterial pathogenicity because they are highly antigenic. There are 4 main types of flagella:
- Monotrichous (one polar flagellum)
- Lophotrichous (several polar flagella),
- Peritrichous (flagella distributed on the entire surface of the cell)
- Amphitrichous (one flagellum located at both ends of the cell.)
Pili
They are also called Fimbriae and play an important role in the adherence of bacteria on the host, a step that is needed for a bacteria to cause infection. Sex pili are involved in Conjugation, i.e., the transfer of DNA between bacterial cells.
Bacterial Spores
Some bacteria species form spores when they are exposed to environmental conditions that are not ideal for growth, such as nutritionally deficient conditions. Spores are highly resistant dormant of bacteria such as Bacillus and Clostridium species.
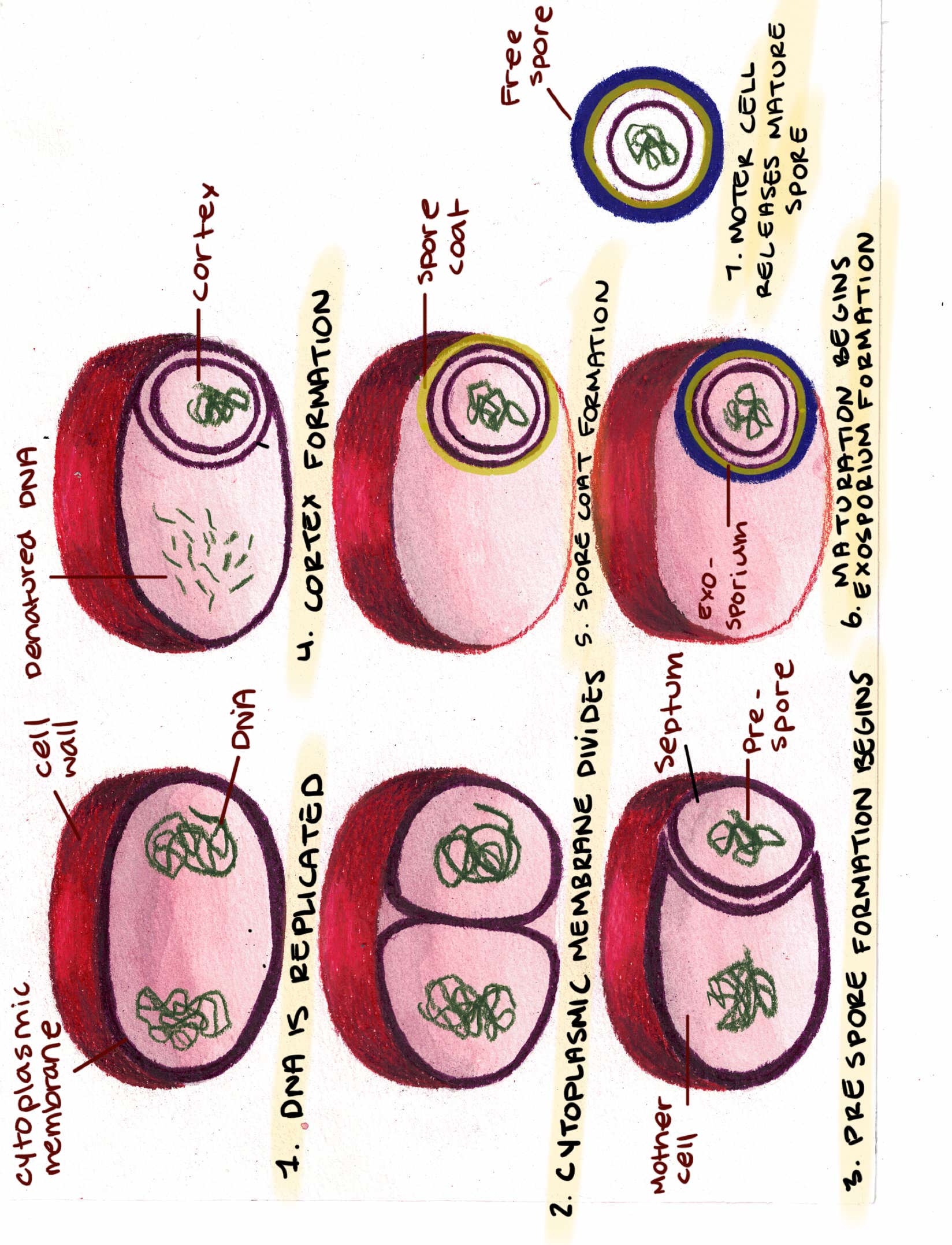
An illustration of the sporulation process.
Bacterial spores are resistant to extreme environmental conditions including boiling, heating, disinfectants, freezing and drying. However, they can be destroyed by autoclaving at 121oC.
The conversion of a spore to a vegetative form is called germination.
Spores can be observed under a microscope as refractile bodies as shown here observed under phase-contrast microscopy.
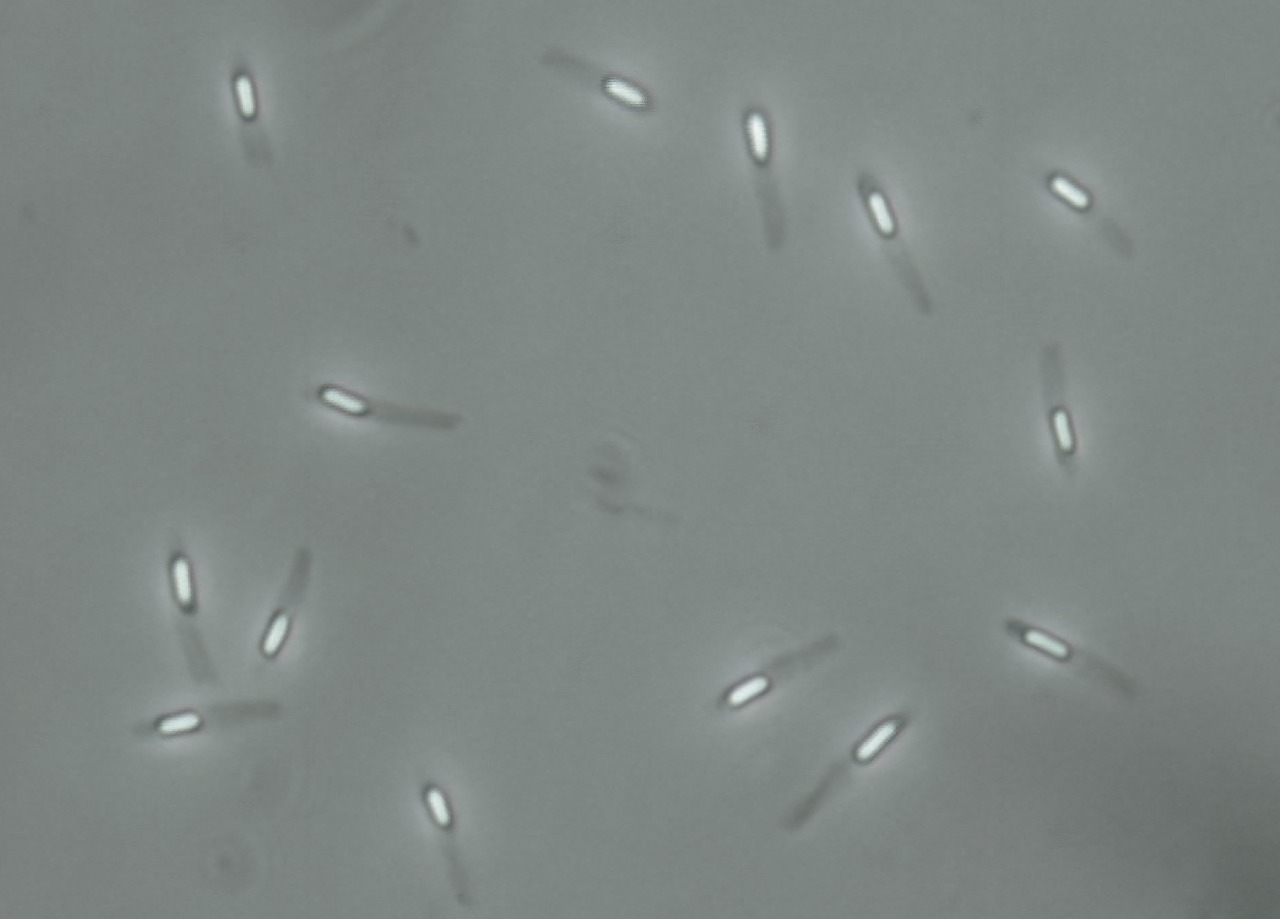
Source: Wikipedia - Under the Creative Commons licence - No alterations made.
Spores can also be observed through gram staining or by using malachite green stain.
Bacterial Growth and Multiplication
Bacterial growth is simply the increase in all the chemical components of the cell. Multiplication occurs when the cell components reach a maximum level. Bacterial growth is expressed as the exponential increase in the number of cells. And the growth rate is the change in the number of bacterial cells per unit time. The Generation time can be defined as the amount of time it takes for a bacterium to give rise to 2 daughter cells. Most pathogenic bacteria have a generation time of about 20 minutes. Mycobacterium tuberculosis has a generation time of 20 hours, while Mycobacterium leprae has one of the longest generation times of 20 days. Because of the exponential nature of the division, an E. coli cell can undergo 30 generations in 10 hours resulting in 1 billion cells
Bacterial Growth Curve
The bacterial growth curve (increase in cell count) shows 4 distinct phases:
- Lag Phase: The cell multiplication does not start immediately when the cells are introduced into the media. and even when the cells start to multiply, there are fewer parent cells, so the increase in number is slower.
- Log phase: This phase is characterized by exponential increase in bacterial cell numbers.
- Stationary phase: This occurs when the cells have exhausted all the nutrients and resources needed for growth. The cells can no longer multiply and the cell numbers remain constant.
- Decline phase: During this phase, the bacterial cell numbers begin to reduce. This is mostly caused by the accumulation of toxic waste and the unavailability of nutrients.
Effects of Oxygen on bacterial growth
The effects of oxygen on bacterial growth depends on whether the bacterial utilize oxygen in their metabolism or not. Bacteria can be classified into:
- Obligate aerobes: can grow only in the presence of oxygen.
- Facultative aerobes: ordinary aerobes but can also grow without oxygen.
- Microaerophilic bacteria: can grow in the presence of low oxygen and in the presence of low concentration of carbon dioxide
- Anaerobic bacteria (also defined as Obligate anaerobes) are the bacteria that can only grow in the absence of oxygen
Other factors that influence bacterial growth include:
- Carbon dioxide levels: Some bacteria, such as Brucella abortus can only grow in conditions with about 10% carbon dioxide. These are called capnophilic bacteria
- Temperature: Bacteria can grow in diverse ambient temperatures such as:
- Psychrophiles: These bacteria are cold loving microbes that grow within a temperature range of 0-20oC.
- Mesophiles: These are moderate temperature loving microbes that grow between 25oC and 40oC. Most of pathogenic bacteria belong to this group.
- Thermophiles: These are heat loving microbes. They can grow at a high temperature range of 55-80oC.
- pH: Most pathogenic bacteria grow between pH 7.2 and 7.6. Very few bacteria, such as lactobacilli, can grow at acidic pH below 4.0. Most foods are preserved by lowering the pH (create acidic conditions).
- Light: Bacteria may be classified as phototrophs (derive energy from light) or chemotrophs (derive energy from chemical substances.
- Osmotic pressure: microbes obtain their nutrition from the surrounding solution so the osmotic pressure has significant influence on the movement of solutes and solvents in and out of the bacterial cell. This explains the technique of preservation using high amounts of salt.
- Moisture: Bacteria grow better under moist conditions. Moisture influences osmotic pressure and also influences the movement of fluids especially outside the bacterial cell. The technique of drying food as a preservation method to inhibit the growth of bacteria is commonly practised all over the world.
Bacterial Nutrition
Bacteria require an energy source such as glucose. They also require sources of elements such as Nitrogen and sulfur (they use to synthesize proteins, DNA, RNA and ATP. Several other elements/ions are needed for normal functioning of the bacterial cells including K, Na, Ca, Fe, Cl, H, C etc. C and H is usually obtained from inorganic compounds supplied in the media. Other bacteria can only grow in media that contain blood, or meat digests or certain supplementary amino acids. Finally, some bacteria, such as Mycobacterium leprae can only grow if inoculated into living animals, they cannot grow in any in vitro cultures.
Sterilization and Disinfection
Microorganisms can cause food spoilage and diseases, so it is necessary to develop ways to inhibit their growth.
Sterilization is defined as the elimination of all living microorganisms including spores. Materials that have undergone sterilization are described as Sterile.
Disinfection is the process of using a chemical (disinfectant) to destroy all pathogenic microbes excluding spores. Disinfectants are used only in inanimate objects. Antiseptics are substances that can be applied directly on the body surface such as skin, wounds, mucous membranes, to inhibit the growth of pathogenic microbes.
Sepsis is defined as the presence of microbes or microbial toxins in the body or in the blood and other tissues. Procedures that prevent the access of microbes into tissues is called Asepsis.
Sanitization defines techniques that mechanically remove microbes along with other organic contaminants. This process is achieved using sanitizers, which include soaps and detergents.
Sterilization
Sterilization can be achieved by two major approaches, using physical (such as sunlight, dry heat, moist heat, filtration, radiation, and sound waves) or chemical processes.
1. Sunlight: Direct sunlight works due to the presence of ultraviolet and heat rays. Its the natural method that reduces the microbial growth in lakes, rivers, and tanks.
2. Moist Heat: Heat is the most common and reliable method of sterilization. High temperatures are microbicidal (they kill the microbes) while lower temperatures (such as freezing) are microbistatic (inhibit microbial growth but do not kill the microbes). Heat sterilization can be through the following techniques:
- Moist sterilization at less than 100oC, as commonly done during pasteurization of liquid beverages such as wine and milk. This technique doesn't kill spores and thermoduric species such as Lactobacilli, Micrococci and Yeasts. So Milk is not sterile after pasteurization. The flash method uses 72oC for 15-30 seconds, followed by rapid cooling to 13oC. Another method uses 134oC for 1-2 seconds (Ultrahigh Temperature - UHT) and results in sterilization. UHT milk can last about 3 months and does not need to be refrigerated.
- Moist sterilization at 100oC: Simple boiling for 10-30 minutes kills most vegetative microbes. Exposing objects to boiling water for the same period also kills most pathogenic vegetative microbes. Because boiling does not kill spores, this technique does not achieve sterilization, and recontamination can occur immediately after the objects are removed from boiling water.
- Moist sterilization at temperatures above 100oC: To achieve temperatures above 100oC, you need to increase the pressure of the container. This can be achieved by using a kitchen pressure cooker, or by using an autoclave. Experience has shown that the most efficient pressure and temperature combination for achieving sterilization by autoclave is 15 psi, which yields 121°C for between 10 - 40 minutes depending on the size of the load.
3. Dry Heat: There are several processes that use dry heat for sterilization. The advantage is that one is not limited to water's boiling point, dry heat can achieve up to several thousand oC.
- Dry sterilization by flaming: usually used in microbiology when inoculating microorganisms into different culture media using the inoculating loop.
- Dry sterilization by incineration: This technique is used to totally destroy biological material that may have been contaminated by microbes, especially when there is a possibility of spore formation. Such as anthrax carcasses. Its also used for most hospital waste, pathology samples, dressings, bandages etc.
- Dry sterilization using the hot air oven: this is the most common method, using temperatures around 160oC. The objects should be dry and will need to be exposed for 2.5 hours.
3. Filtration: Solutions that cannot be heated can be sterilized through filtration. They can be used to sterilize pharmaceutical substances, ophthalmic solutions, liquid culture media, oils, antibiotics, and other heat-sensitive solutions. Filtration can also be used to obtain bacteria-free filtrates of samples/specimens for virus isolation. Air can also be sterilized by filtration such as using HEPA filters to remove nearly 99% of particles from the air.
4. Radiations: Both ionizing and non-ionizing radiations can be used to sterilize objects. X-rays, Gamma rays, Cosmic rays all have microbicidal effects and can also destroy spores. Non-ionizing radiations such as UV radiation is used primarily for disinfection of closed areas in microbiology laboratory, inoculation hoods, laminar flow, and operating theaters. It kills most vegetative bacteria but not spores, which are highly resistant to these radiations. However, it does not penetrate glass, dirt films, water, and other substances very effectively.
5. Sound waves: High frequency sound waves can generate heat that has antimicrobial action. Gram-negative rods are most sensitive to ultrasonic vibrations, while Gram-positive cocci, fungal spores, and bacterial spores are resistant.
Disinfection
We have already defined a disinfectant, but what are the properties of an ideal disinfectant:
- Should have a broad spectrum of activity i.e., be effective against a wide variety of microbes.
- It should retain efficacy in the presence of organic matter such as feces, blood etc.
- It should not be toxic to human or corrosive.
- It should be stable during storage and should not undergo chemical changes.
- It should be odorless or with a pleasant odor.
- It should be soluble in water and/or lipids for penetration into microorganisms.
- It should be effective in surfaces with varying pH levels.
- It should act fast .
- It should be relatively inexpensive and easily available.
Factors influencing the efficacy / activity of disinfectants:
- Temperature: high temperatures usually increase the efficacy.
- Types of microbes present
- Physiological state of the microbial cells, with physiologically active cells being more susceptible.
- Environment: This encompasses factors like pH, presence of organic material, surface material characteristics, presence of other disinfectants etc.
The various types of disinfectants include:
- Phenolic compounds such as Phenol and Cresol.
- Halogens such as Iodine: used in surgeries, preventing mastitis, mouth wash etc.
- Alcohols: At about 70% can be used as a disinfectant and antiseptic.
- Aldehydes: such as Formaldehyde is microbicidal, sporicidal, and can also kill viruses.
- Heavy metals: such as Copper Sulfate used as a footbath to prevent viral and bacterial infections entering into livestock farms, or Copper sulfate used as disinfectant in swimming pools.
- Oxidizing agents: such as hydrogen peroxide is used in wound treatment such as abscesses, and also in used in mouth wash.
- Dyes: such as Gentian violet (GV) are popular for wound treatment. They are more effective against gram positive bacteria than gram negative bacteria.
- Acids and Alkali: All living cells have a narrow range of optimum pH that allows optimal growth. changing the pH of the surface can have inhibitory effects on microbial growth.
Bacterial Cultures
Cultures are a way to confirm the presence of specific bacterial species in a sample. It is most commonly used to confirm the causative agent of a disease. Bacterial cultures can either be solid or liquid (broth). KIch pioneered the use of agar as a base for culture media. Agar is an ideal base because it doesn't melt until it is exposed to temperatures above 100oC, and also because it is not metabolized by most bacteria. Agar is obtained from a variety of sea weeds and is processed into powder.
Other ingredients in bacterial cultures include:
- Peptone: a mixture of partially digested proteins
- Water
- Sodium Chloride
- Electrolytes
- Extracts of yeast, meat, malt, blood or serum.
Liquid Media
Bacteria grown in liquid media form colloidal suspensions and need to be sub cultured onto solid media to be able to process the colonies for identification. Growth in liquid media cannot be quantified since it doesn't occur as separate colonies.
Solid Media
Uses agar as the solidifying agent. Some bacterial species can be recognized based on colony morphology.
Nutrient agar is the simplest and most common type of growth agar. It is prepared by adding 2% agar to a nutrient broth. Other examples of solid media include Blood agar, Chocolate agar, MacConkey agar and others.
Semi-Solid agar Is made using a lower concentration of agar. Semi-solid media allow bacteria to spread more easily in the media.
Enrichment Media is a liquid media that stimulates the growth of certain bacteria or suppress the growth of others. Enrichment media is used when culturing specific bacterial species from samples that are expected to have too many bacterial species. For example, if you intend to isolate E coli from a sample of feces, which has many other bacterial contamination.
Selective Media: contain substances that inhibit the growth of certain bacterial species. For example.
- Thiosulfate citrate bile salt sucrose agar (TCBS) selective for the isolation of Vibrio cholerae.
- Deoxycholate citrate agar (DCA) selective for enteric bacilli, such as Salmonella spp. and Shigella spp
Differential or indicator media: used to distinguish one microorganism from another growing on the same media by their growth characteristics.
Transport media: Transport media is used to maintain the viability of certain delicate organisms in clinical specimens during their transport. The media doesn't contain nutrients as such, it contains mostly buffers and salt.
Sugar Media: Sugar media contains low concentrations of sugar (about 1%). The sugar used may be sucrose, glucose, or lactose. Sugar media is used to detect if fermentation has occurred. The fermentation products are detected using an indicator (usually Andrade's indicator.
Culture Techniques
There are several techniques that can be used for culturing, as follows
- Streak Method: This technique is useful for obtaining discrete colonies of bacteria.
 Image source, Wikipedia, under the Creative Commons licence. No modifications made.
In this method, a loopful of bacterial inoculum is placed close to the periphery on the surface of the agar, then spread with the loop using close parallel strokes. Further parallel strokes are made with the loop starting from the primary inoculum as shown in the figure.
Image source, Wikipedia, under the Creative Commons licence. No modifications made.
In this method, a loopful of bacterial inoculum is placed close to the periphery on the surface of the agar, then spread with the loop using close parallel strokes. Further parallel strokes are made with the loop starting from the primary inoculum as shown in the figure. - Lawn Culture: This technique is aimed to produce a uniform layer of bacterial growth on a solid medium. The liquid culture is poured on the surface of the plate with the excess pipetted out. Then incubated overnight.
- Pour-Plate Culture: This technique is performed by mixing a liquid sample containing bacteria into molten agar and the mixture is agitated to distribute the sample throughout the a=molten agar. The mixture is then poured onto a petri dish and incubated overnight. Bacterial colonies will be observed spread out throughout the depth of the agar and can be counted. This technique is suitable for estimating the number of viable bacteria in a liquid sample such as urine.
- Stab Culture: The culture is added to the agar by stabbing using a long straight wire.
Bacterial Taxonomy
In addition to microscopy, discussed here, bacteria maybe identified using their colony characteristics and biochemical reactions.
Colony Morphology
- Colony size: pinhead size (Staphylococcus aureus) or pinpoint (streptococci).
- Colony Shape: May be circular or irregular, and surface of the colonies may be smooth, rough, or granular.
- Colony surface may be flat, raised, low convex, convex, or umbonate.
- The colony edge may be entire, lobate, crenated, undulate, or ciliate.
- The colonies may be transparent, translucent, or opaque.
- Some bacterial species produce pigment, which can be detected ac the colored colonies. Some other species produce products that cause hemolysis which can be detected when grown on blood agar.
Biochemical Reactions
- Catalase Reaction: The Catalase enzyme breaks down hydrogen peroxide and releases oxygen. The catalase test is used to differentiate Staphylococcus and Streptococcus. A small amount of culture is picked up from the agar plate and is inserted into hydrogen peroxide solution. Production of bubbles indicates a positive reaction.
- Urease Test: This test is used to determine the ability of bacteria to split urea into ammonia. Phenol red is used as an indicator because production of ammonia makes the medium alkaline and therefore turns red or pink in color.
- Citrate test: The citrate test is used to determine if an organism can utilize citrate as the only source of carbon for metabolism.
- Methyl red test: The methyl red test determines the ability of a bacteria to produce and maintain stable acid products during the fermentation of glucose.
- Hydrogen sulfide test: This test is used to determine if the bacteria produce hydrogen sulfide. The media needs to contain sulfur, for example lead acetate or ammonium acetate medium. Hydrogen sulfide is produced by the metabolism of sulfur containing amino acids.
- Other biochemical tests include:
- Animal Pathogenicity tests
- Antibiotic sensitivity tests
- Assessment of antigenic structures
Bacterial typing
Bacterial is the use of different assays and observable properties to classify bacteria. Some types of typing include:
- Biotyping: Utilizes several biochemical tests to distinguish various bacterial strains.
- Serotyping: This technique utilizes the expression of different antigenic determinants on the surface of the cell.
- Bacteriocin typing: This is used in bacterial species where several lytic bacteriophages have been identified.
- Phage typing: This is the most widely used method and utilizes the specificity of the bacteriophages that bind to the bacteria.
Microbial Nomenclature
Tha naming of microbes is governed by the International Committee on Systematic Bacteriology. The nomenclature of viruses is governed by the International Committee on Taxonomy of Viruses.
Microbes usually have two names: the common name and scientific name. The common name is regional specific and might differ in different languages. The scientific name is internationally recognized and remains the same throughout the world. The order name end with -ales, the family name ends in -eceae and the tribe's name ends in -eae. As in other taxonomic systems, the genus name starts with an upper case but species name starts with lower case. the genus and species names are either in italics or underlined. When the name is mentioned for the first time it is written in full, but subsequent mentions in the text can be abbreviated.
Bacterial Genetics
Unlike eukaryotes, bacteria are haploid (1n), indicating that they have a single copy of each gene.
Bacterial Transformation
Bacterial transformation occurs when a cell takes up DNA found in the environment and incorporates it into its genome. Nore that. not all bacteria can be transformed, and not all extracellular DNA is able to cause transformation. To be competent to be transformed, the bacterial cell needs to have a surface protein called Competent Factor, which binds to the extracellular DNA in an energy requiring reaction. Bacteria that are not naturally competent can be treated to make them competent, usually by treatment with calcium chloride, which makes them more permeable.
Bacterial Conjugation
Bacterial conjugation is the transfer of genetic material (plasmid) between bacterial cells by direct cell-to-cell contact or by a bridge-like connection between two cells. Bacterial conjugation is considered as the bacterial equivalent of sexual reproduction or mating since it involves the exchange of genetic material. Most conjugative plasmids have systems ensuring that the recipient cell does not already contain a similar element.
Bacterial Transduction
Is the movement of DNA between two bacterial cells mediated by a bacteriophage.
DNA Transfer Within the Bacterial Cells
There are three processes that enable transfer of DNA to occur within the bacterial cell; Transposons, Integrative Conjugative Elements and Programmed Rearrangements.
1. Transposons: Transposons are a type of mobile DNA elements of 2000-20,000 bases long. They can transfer DNA from one site of the bacterial chromosome to another site or to a plasmid. These have also been named jumping genes and the process is called Transposition.
2. Integrative Conjugative Elements (ICEs): ICEs are ways of horizontal gene transfer and self transmissible mobile genetic elements.
3. Programmed Rearrangements: This involves the movement of a gene from a silent site (where the gene is not expressed) to an active site. Many silent genes code for variants of antigens and these movements results in new antigenicity and antigenic variation.
Bacterial Recombination
After DNA has been transferred, it combines with the chromosomal DNA by a process called recombination. Recombination can be homologous or nonhomologous. Homologous recombination occurs when the DNA pieces show extensive homology. As expected, nonhomologous recombination occurs when the two DNA fragments show little or no homology.
Microbial Biotechnology
This section will cover techniques that deliberately modify an organism's genetic information by changing its genome.
Genetic Engineering
Genetic engineering is the application of genetic tools to tackle social needs. An organism that is generated through genetic engineering is genetically modified (GM) and the resulting product is a genetically modified organism (GMO). If genetic material from another species is added to the host, the resulting organism is called transgenic. If genetic material from the same species or a species that can naturally breed with the host is used the resulting organism is called cisgenic. The DNA fragment can be introduced directly into the host organism or into a cell that is then fused or hybridised with the host.
Microbial Pathogenicity
Types of Microorganisms
Microorganisms can be classified into 5 groups based on their interaction with their host.
- 1. Saprophytes: Saprophytes are free living microbes that live on dead and decaying material. They are present in soil and water and are usually unable to invade humans or animals to cause disease.
- 2. Parasites: These microbes live on a living host, deriving their survival from them, but causing harm to the infected host.
- 3. Pathogens: These microbes cause disease in the host. Only a small proportion of the microbial population can be 'pathogens'.
- 4. Commensals: These microbes live on a living host but do not cause any harm to the host. They represent a large proportion of the microbes present in humans and animals.
- 5. Opportunistic pathogens: These are microbes that can cause disease only in immunocompromised people, or when there is an imbalance of the microbial ecosystem.
Pathogenicity is defined as the capacity of a pathogen to cause disease. Pathogenicity should be differentiated from virulence, which refers to the sum of disease-causing properties of the strain/population of pathogens. Pathogens have gene clusters called pathogenicity islands that are associated with their disease-causing properties.
Stages of Pathogenesis
A pathogen can cause disease in a host (or multiple hosts) is it is able to:
- Break the host defence barriers.
- Replicate within the host and spread to different organs/tissues.
- Spread to new susceptible hosts.
- Overcome the ability of the host to eliminate the microbes.
Types of Infections
There are several ways to categorise infections based on multiple factors
- Primary infection: As the term suggests, a primary infection is the initial infection of a host by a pathogen.
- Reinfection: When a host is infected by the same organism a second or multiple times.
- Secondary Infection: When one organism makes it easier for another organism to infect the host. The other organism is considered the secondary infection. It wouldn't have occurred in the absence of the initial pathogen.
- Cross infection: Occurs when a new organism, from another host, infects a host/patient who is already suffering from another disease.
- Nosocomial Infection: These are cross infections that are acquired in hospital.
- Iatrogenic Infection: These are infections that are induced by a physician as a result of therapy with drugs or other diagnostic investigations.
- Subclinical infections: Infections that are present in a host but do not cause manifestations of signs/symptoms of disease.
- Latent infection: A infection where the pathogen remains in a latent state and begins to multiply and cause disease when the host immune responses are lowered.
Modes of Transmission
Transmission simply denotes the spread of an infection to a new host. There are 6 major modes of transmission of diseases.
- 1. Contact: Diseases such as common cold can be transmitted through direct contact between infected individuals. Sexually transmitted diseases are also considered in this category since they are successfully transmitted when there is direct contact. Pathogens can also be transmitted through indirect contact through objects such as toys, clothing etc. These objects are called fomites. Diseases such as influenza can be transmitted through fomites.
- 2. Inoculation: Diseases such as tetanus are introduced into the body when an individual is injured with sharp objects. Tetanus organisms (Clostridium tetani) occur as spores on metal objects that have been contaminated by soil or rust. The spores germinate to vegetative form when they enter the are inoculated into the body and the bacteria then migrate into nervous tissue causing the classical signs of tetanus. As mentioned previously, iatrogenic infections are caused by introducing pathogens during injection or by other equipment in a hospital. Hepatitis B and C and HIV are examples of iatrogenic infections.
- 3. Ingestion: Ingestion of water or food contaminated with microbes can be a route of transmission of infections. Cholera, typhoid, and many parasitic diseases (such a amoeba and giardia) can be transmitted by drinking contaminated water.
- 4. Inhalation: Droplets containing pathogens can be discharged by an infected host trough coughing, sneezing, or talking. Depending on the pathogen, the droplets can remain viable for a long period of time. These small droplets could be inhaled by a susceptible host and cause disease. Influenza, whooping cough and tuberculosis -TB are some examples of diseases that can be transmitted through droplets.
- 5. Vectors: Vectors are living things (as compared to fomites that are non-living things) that carry pathogens, they themselves do not get infected by the disease but they transmit the pathogens to susceptible hosts. Mosquitoes are probably the best example of vectors, but ticks, fleas, mites, lice etc. are vectors for various pathogens.
- 6. Vertical Transmission: Vertical transmission occurs when pathogens are transmitted from a mother to her fetus either in utero or through breast milk. All routes of disease transmission that occur between person to person but not from mother to offspring can be grouped as horizontal transmission.
Stages of Disease Progress
There a 4 stages of disease progression:
- Incubation period: This is the period between entry of the pathogen to the onset of clinical signs of disease. This is the time it takes for the pathogen to multiply.
- Prodrome period: The period during which only non-specific disease symptoms occur.
- Specific symptoms period: This period is characterized by symptoms that are more specific to the disease.
- Recovery period: During this period, the disease symptoms resolve and the patient gains normal health.
Depending on epidemiological factors, diseases can be classified as
- Endemic: These diseases are of low prevalence and occur in specific geographical areas but are persistent.
- Epidemic: Epidemics occur in specific geographical areas but at a much higher prevalence rate.
- Pandemic: Pandemics occur at a higher prevalence rate and spread over much larger areas of the world.
Antimicrobials - Use and Resistance
Antimicrobials are substances that have the ability to kill or inhibit microorganisms.
Antibiotics are substances produced by the natural metabolic processes of some microorganisms that can inhibit or destroy other microorganisms.
Antimicrobials can be categorised according to the spectrum of activity:
1. Broad-Spectrum are also called 'Extended-spectrum' antimicrobials are active against a wider range of microbes. Tetracyclines are a good example as they work against various gram-positive and gram-negative bacteria and are also effective against mycoplasmas, protozoa and rickettsia.
2. Narrow Spectrum antibiotics are effective against one or very few microbes. Vancomycin is an example as its effective against gram-positive bacteria such as staphylococci and enterocci.
Antimicrobials may also be bactericidal- which kill the bacteria or bacteriostatic - which inhibit growth/multiplication of the bacteria.
Mechanisms of Action of Antimicrobials
1. Inhibition of Cell Wall Synthesis:
Antibiotics such as Penicillins, Cephalosporins and Vancomycin interfere with cell wall synthesis. Penicillins and Cephalosporins are referred to as beta-lactam antibiotics because they possess a beta-lactam ring, which is essential for the antimicrobial activity.
- Penicillins
Penicillins are a group of bactericidal drugs in the beta-lactam group. They contain a 6-aminopenicillanic acid nucleus that contains the beta lactam ring. They act primarily on gram-positive bacteria. Other penicillins such as Ampicillin, Amoxycillin, Piperacillin, Carbenicillin, Ticarcillin etc. are effective against both gram-positive and gram-negative organisms. - Cephalosporins
Cephalosporins, like penicillins, are also beta-lactam antibiotics, however, in contrast, they have a 7-amino-cephalosporanic acid instead of 6-aminopenicillanic acid. Cephalosporins are grouped into First generation and second, third and fourth generation. First generation cephalosporins are effective against mainly gram-positive bacteria. The second, third and fourth generation cephalosporins are effective against gram-negative bacilli.
Some examples of cephalosporins are:
a. First generation: Cephalexin, Cephalothin, Cephradine and Cephaloridine.
b. Second generation: cefaclor, cefuroxime, Cefoxitin, cefmetazole.
c. Third generation: Cefoperazone, Cefotaxime, cefixime etc.
d. Fourth generation: Cefpirome and cefepime. - Vancomycin
Vancomycin is a glycopeptide but works in a very similar way as beta-lactam antibiotics. Vancomycin kills bacteria - bactericidal- by inhibiting cell wall synthesis. Vancomycin is used:
a. Against Staphylococcus spp and Clostridium spp.
b. Colitis
c. Treatment of methicillin resistant Staphylococcus aureus infections. - Teicoplanin
Teicoplanin is a glycopeptide extracted from Actinoplanes teichomyceticus and has a similar antimicrobial spectrum as Vancomycin. Teicoplanin is used:
a. Prophylaxis and treatment of infections caused by Gram-positive bacteria, methicillin resistant staph and Enterococcus faecalis.
b. Treatment of colitis and Clostridium difficile associated diarrhea.
2. Inhibition of Protein Synthesis:
Because of the differences between bacterial and eukaryotic ribosomes, antimicrobials that prevent protein synthesis in bacteria do not affect protein synthesis in mammals. Aminoglycosides and Tetracyclines act at the 30S subunit, while Erythromycins, Chloramphenicol and Clindamycins act at the 50S ribosomal subunit.
- Aminoglycosides:
These are a family of antimicrobials that include Streptomycin, Gentamycin, Neomycin, Tobramycin and Amikacin. - Tetracyclines:
This is a family of drugs that include dimethylchlorotetracyclines, doxycycline and rolitetracycline. they are bacteriostatic and their action is reversible when the antibiotic is withdrawn. They are effective against cocci and bacilli. They are also effective against chlamydial and rickettsial infections. - Macrolides
Macrolides include Erythromycin, Azithromycin, Clarithromycin and Roxithromycin. They are bacteriostatic and contain a macrolide ring with attached sugars. Erythromycin is effective against gram-positive cocci including methicillin resistant Staph aureus and Haemophilus influenzae. - Chloramphenicol
Chloramphenicol is bacteriostatic and growth of bacteria resumes when the antibiotic is not administered. It binds to the 50S ribosomal subunit and blocks the addition of amino acids to the peptide chain. - Clindamycin
Clindamycin inhibits protein synthesis by blocking the release of t-RNA after it has transferred an amino acid to the growing peptide.
3. Inhibiting Nucleic Acid Synthesis:
Antimicrobials that block nucleic acid synthesis include - Sulfonamides, Trimethoprim, Quinolones and Rifampin.
- Sulfonamides and Trimethoprim
Sulfonamides are similar in chemical structure to Para-aminobenzoic acid (PABA) so sulfonamides compete with PABA during the microbe's metabolism. The folic acid formed as a result doesn't function normally, thereby resulting in the inhibition of bacterial growth. This mechanism makes them bacteriostatic. Sulfonamides are effective against Gram-negative and Gram-positive bacteria.
Trimethoprim inhibits the dihydrofolic acid reductase enzyme which reduces dihydrofolic acid reductase to tetrahydrofolic acid, leading to reduced synthesis of purines. - Quinolones
Some examples of quinolones include Ciprofloxacin, Ofloxacin and Levofloxacin. Quinolones are bactericidal synthetic analogs of nalidixic acid and act by inhibiting DNA synthesis by blocking the gyrase enzyme, which unwinds DNA strands before replication. They are effective against both gram-positive and gram-negative microbes. - Rifampin
Rifampin binds to the DNA dependent RNA polymerase of bacteria inhibiting RNA synthesis. It has the ability to block assembly of poxviruses.
4. Altering Cell Membrane Function:
Some common examples of antimicrobials that alter cell membrane functions include Amphotericin B and Azoles, which are commonly used antifungals. Azoles include Ketoconazole, Fluconazole, Clotrimazole.
Polymyxin B is an antibiotic used in resistant Gram-negative bacteria. It is bactericidal because it binds to the cell membrane and makes it more permeable, water moves into the cell and causes lysis. It is effective against all Gram-negative bacilli except those on the proteus group. It is commonly used in topical preparations.
Antimicrobial Resistance
A more detailed review of this topic is available in our pharmacology course.
Antibiotics resistance is observed in hospital acquired infections more frequently such as hospital strains of Staphylococcus aureus and some E. coli strains. These strains of bacteria possess resistance to multiple antimicrobials. Resistance genes are usually located in plasmids.