Course Detail
Mycology
List of Contents
General Introduction
Mycology is the branch of biology concerned with the study of fungi, including their genetic and biochemical properties, their taxonomy and their use to humans as a source for tinder, traditional medicine, food, and entheogens, as well as their dangers, such as toxicity or infection.
Previously, mycology was a branch of botany because, although fungi are evolutionarily more closely related to animals than to plants, this was not known until more recently.
Fungi are essential for life on earth in their roles as symbionts, e.g. in the form of mycorrhizae, insect symbionts, and lichens. Many fungi are able to break down complex organic biomolecules such as lignin, and pollutants such as xenobiotics, petroleum, and polycyclic aromatic hydrocarbons. By decomposing these molecules, fungi play a critical role in the global carbon cycle.
Fungi are also often economically and socially important, as some cause diseases of animals, humans and of plants. In addition, many fungal species are very important in controlling the plant diseases caused by different pathogens. For example, species of the filamentous fungal genus Trichoderma are considered one of the most important biological control agents as an alternative to chemical-based products for effective crop diseases management. Mushrooms produce large amounts of vitamin D when exposed to ultraviolet (UV) light.
Some fungi produce toxins, antibiotics and other secondary metabolites. For example, the genus Fusarium and their toxins associated with fatal outbreaks of alimentary toxic aleukia in humans. Penicillin, ciclosporin, griseofulvin, cephalosporin and psilocybin are examples of drugs that have been isolated from molds or other fungi.
The fungi are eukaryotic organisms and they differ from the bacteria, which are prokaryotic organisms, in many ways. For instance, fungi possess rigid cell walls, which possess two characteristic cell structures: chitin and ergosterol. Chitin is a polysaccharide consisting of long chains of N-acetylglucosamine. In addition to chitin, the fungal cell wall also contains mannan and other polysaccharides. Of these, beta-glucan is most important, because it is the target of antifungal drug caspofungin. Unlike human cell membrane which contains cholesterol, fungal cell membrane contains ergosterol. This difference resulted in the development and efficacy of antifungal agents such as amphotericin B, fluconazole, and ketoconazole.
Differences between Bacteria and Fungi
| Characteristic | Fungi | Bacteria |
|---|---|---|
| Diameter | Approximately 4 µm | Approximately 1 µm |
| Morphology | Yeast and mold | Cocci, bacilli, spirochete, branching filamentous |
| Staining properties | Gram-positive, nonacid fast, stained with PAS and GMS | Gram-positive, Gram-negative, acid fast |
| Cell wall content | Chitin | Peptidoglycan |
| Cell Membrane | Sterols present | Sterols absent except mycoplasma |
| Cytoplasm | Mitochondria and endoplasmic reticulum present | Mitochondria and endoplasmic reticulum absent |
| Nucleus | Eukaryotic | Prokaryotic |
| Spores | Sexual and asexual spores for reproduction | Endospores for survival, not for reproduction |
| Thermal dimorphism | Yes (observed in some fungi) | No |
Morphological Classification
The fungi can be classified into the following four main groups based upon the morphology: (a) yeast, (b) yeast-like form, (c) molds, and (d) dimorphic fungi.
Yeast: Yeasts are round or oval unicellular fungi that reproduce by asexual budding. On culture medium, such as Sabouraud's dextrose agar (SDA), they produce creamy mucoid colonies. Example: Cryptococcus neoformans.
Yeast-like fungi: These are the yeasts with pseudohyphae. Example: Candida albicans.
Molds: Molds grow as long filaments called hyphae. They usually measure 2-10 µm in width. Some hyphae form transverse walls and hence they are called septate hyphae, whereas others do not produce walls, hence are called nonseptate hyphae. Nonseptate hyphae are multinucleated. The hyphae on their continuous growth form a mat known as mycelium. The part of the mycelium that projects above the surface in culture medium is called aerial mycelium. Examples include Aspergillus, Penicillium, Rhizopus, etc.
Dimorphic fungi: Many of medically important fungi are dimorphic. They exist as hyphal/mycelial forms in the soil and in the cultures at 22-25oC. They occur as yeasts or other structures in human tissue and in the culture at 37oC. Examples include Coccidioides immitis, Paracoccidioides brasiliensis, Histoplasma capsulatum, Blastomyces dermatitidis, and Sporothrix schenckii.
Taxonomic Classification
Fungi are placed in the phylum Thallophyta. There are four classes of fungi: Zygomycetes, Ascomycetes, Basidiomycetes, and Deuteromycetes or Fungi Imperfecti.
Reproduction in Fungi
Fungi can reproduce sexually by forming sexual spores and asexually by forming conidia or asexual spores. Sexual spores are of three types: zygospores, ascospores, and basidiospores. Ascospores are formed in a sac called ascus, whereas basidiospores are formed outside on the tip of a pedestal called a basidium. Zygospores are single, large spores with thick wall. The fungi that do not produce sexual spores are called imperfect and are classified as Fungi imperfecti. Asexual spores are produced by mitosis. Fungi reproduce asexually by forming conidia. The shape, color, and arrangement of the conidia are helpful for identification of the fungi.
A. Vegetative spores include:
- Arthrospores
- chlamydospores
- blastospores
Arthrospores are formed by fragmentations of the ends of hyphae, resulting in rectangular thick-walled spores. The arthrospores are the infective stage of C. immitis.
Chlamydospores arise by rounding and thickening of hyphal segments. They are round and thick walled. The terminal chlamydospores help in the identification of C. albicans.
Blastospores are formed by budding process from parent cells, such as yeast. Some yeasts, such as C. albicans can form multiple buds that do not detach from the parent yeast, thus producing elongated structures called pseudohyphae.
B. Aerial spores include:
- Sporangiospores
- Conidiospores
- Microconidia
- Macroconidia
Sporangiospores are spores formed within a sac called sporangium, which develops at the ends of the hyphae called sporangiophores (e.g., Mucor and Rhizopus).
Conidiospores, or otherwise called conidia, are spores found externally on the sides or tips of hyphae. Conidia can be macroconidia or microconidia.
Macroconidia are large, aseptate, often multicellular conidia.
Microconidia are small and single.
General Pathegenesis of Fungal Infections
Fungi are ubiquitous in nature, i.e., they occur as free-living saprobes, hence determining their role in human infection may sometimes be difficult.
Most fungi are obligate aerobes or facultative anaerobes, but none are obligate anaerobes. The natural habitat of most fungi is environment, because all these fungi require a preformed organic source of carbon, hence their constant association with decaying matter. C. albicans is exception and is an important fungus, which is a part of the normal human flora.
Cell-mediated immunity is much important in conferring protection against fungi. Suppression of cell-mediated immunity can lead to reactivation and dissemination of asymptomatic fungal infection and to diseases caused by opportunistic fungi. The humoral immunity is mediated by production of IgG and IgM antibody. But their role in protection from fungal disease is uncertain.
The effects of fungi on humans can be grouped in three major ways as follows: (a) colonization and disease, (b) hypersensitive diseases, and (c) diseases caused by mycotoxins or fungal toxins
Fungal infection that occurs in the immunocompromised hosts is called as opportunistic mycosis. If such conditions are not rapidly diagnosed and immediately managed, they can prove to be life-threatening.
- Colonization and Disease: Most fungal infections are mild and self-limited. Intact skin is an effective host defense against certain fungi. But if the skin is broken, organisms, the fungi enter through that broken skin and initiate the infection. Fatty acid content, pH, epithelial turnover, and normal bacterial flora of the skin contribute to host resistance against fungi. For example, the mucous membrane of the nasopharynx traps inhaled fungal spores.
- Hypersensitivity Diseases: Humans are continually exposed to air-borne fungal spores and other fungal elements present in the environment and depending on individual's immunological status may induce a state of hypersensitivity. Rhinitis, bronchial asthma, alveolitis, and various forms of atopy are the clinical manifestations of hypersensitive pneumonitis. The clinical manifestations of the hypersensitivity disease are seen only in sensitized person, after repeated exposure to the fungus, fungal metabolites, or other cross-reactive materials. Allergies to the fungal spores are manifested primarily by an asthmatic reaction including rapid bronchial constriction mediated by IgE, eosinophilia, and positive hypersensitivity skin test reaction.
- Fungal Toxins: ycotoxicosis is caused by ingested fungal toxins. Mycotoxicosis caused by eating amanita mushroom is the best example of mycotoxicosis. Aflatoxin is another fungal toxin produced by Aspergillus flavus that causes disease in humans. Aflatoxin-B causes a mutation in the P53 tumor-suppressor gene, resulting in a loss of P53 protein, thereby in a resultant loss of growth control in the hepatocytes. Hence, it causes damage to liver, and it induces tumor in liver in animals and is associated with hepatic carcinomas in humans. Claviceps purpurea is a mold that infects brain and produces alkaloids, such as ergotamine and lysergic acid diethyl amide. These compounds cause serious vascular and neurological effects.
General Diagnostic Approcahes
Diagnosis of fungal infections can be done using:
- Microscopy
- Culture
- Serology
- Molecular techniques
- Other non-culture methods
Microscopy: The commonly used clinical specimens are sputum, lung biopsy material, and skin scrapings. The specimen is either treated with 10% KOH or stained with special fungal stains. Use of 10% KOH dissolves tissue material, leaving the alkali-resistant fungi intact. This techniques relies on the demonstration of characteristic asexual spores, hyphae, or yeast by light microscopy. The disadvantages of microscopy are that it shows low sensitivity and requires an experienced microscopist for specific identification.
ulture: Fungal culture is a frequently used method for confirming the diagnosis of fungal infection. SDA is the most commonly used medium for fungal culture. Other media include CHROM agar, blood agar, etc. The low pH of the medium and addition of chloramphenicol and cycloheximide to the medium inhibit the growth of bacteria in the specimen and thereby facilitate the appearance of slow-growing fungi. Fungal colony is identified by rapidity of growth, color, and morphology of the colony at the obverse and pigmentation at the reverse.
Serology: Demonstration of the antibodies in patient's serum or CSF is useful for diagnosis of fungal infections, especially in systemic fungal infections. A significant rise of antibody titer in a paired sera sample confirms the diagnosis. Recently, newer tests like ELISA (enzyme-linked immunosorbent assay), Western blot, and radioimmunoassays are increasingly used for serodiagnosis of fungal infections.
Nonculture Methods: These methods include:
- Detection of fungal antigen
- Detection of fungal cell wall markers
- detection of fungal metabolites
Antifungal Drugs
Drugs designed to treat bacteria have no significant effect on fungi. Amphotericin B and various azoles are the most effective antifungal drugs. They act on the ergosterol of fungal cell membrane that is not found in bacterial or human cell membrane. Similarly, caspofungin inhibits synthesis of beta-glucan, which is found only in fungal membrane but not in bacterial or human cell membrane.
Superficial, Cutaneous, and Subcutaneous Mycoses
Depending on the tissues that are initially colonized, fungal infections can be categorized into three groups:
- Superficial mycoses: These are surface infections of the skin, affecting the outermost layers of skin, hair, and mucosa
- Cutaneous mycoses: These are infections of the skin involving the epidermis and its integuments, the hair, and nails.
- Subcutaneous mycoses: These are infections of the dermis, subcutaneous tissue, muscle, and fascia.
Superficial Mycoses
Superficial mycosis is restricted to the outermost layers of the skin and hair and only causes cosmetic problems which can be easily treated. They include: (a) pityriasis versicolor, (b) tinea nigra, (c) black piedra, and (d) white piedra.
Pityriasis (Tinea) Versicolor
P. versicolor is a superficial infection of the skin caused by Malassezia furfur (Pityrosporum orbiculare). M. furfur requires fatty acids for growth, hence is cultured on the Sabouraud's dextrose agar (SDA) overlayed with a layer of olive oil. On incubation at 37oC, the fungus produces creamy colonies within 5-7 days.


They appear as hypopigmented macular lesions often associated with slight scaling or itching. The condition is mostly asymptomatic. It occurs most frequently in hot and humid weather
Laboratory diagnosis of the condition is usually made by demonstration of both budding yeast cell and hyphae in KOH preparation of skin scrapings. Characteristic "spaghetti and meatballs" appearance of fungus is demonstrated in the microscopy of KOH preparation of the skin.
Tinea Nigra
Tinea nigra is an infection of keratinized layer of skin caused
by Exophiala werneckii or Cladosporium werneckii. C. werneckii is a dimorphic fungus that produces melanin. A well-demarcated brown-black macular lesion, which appears as rough, brown or black patch of the skin, is typical manifestation of the condition. These brownish to black lesions are most commonly seen on palms and soles.
 Tinea nigra has a long incubation period. This means that it doesn't show up immediately after you come in contact with the fungus. You'll see color changes in your skin at least 2 to 7 weeks after exposure. People who have excessive sweating, or live near the ocean, have higher chances of getting tinea nigra.
Tinea nigra has a long incubation period. This means that it doesn't show up immediately after you come in contact with the fungus. You'll see color changes in your skin at least 2 to 7 weeks after exposure. People who have excessive sweating, or live near the ocean, have higher chances of getting tinea nigra.
Laboratory diagnosis of tinea nigra is made by microscopy of the KOH preparation of skin scrapings collected from the affected part. Typical darkly pigmented yeast-like cells and hyperfragmented hyphae are demonstrated.
Treatment: Tinea Nigra may clear up on its own, but it's not likely. An antifungal skin cream will clear up your tinea nigra after 2 to 4 weeks of consistent use.
Piedra
Piedra Piedra, which means stone in Spanish, refers to a superficial infection of the hair shaft, which was first described in 1969. Two types of piedra are clinically recognized—white and black piedra, both of which have distinct characteristics. White piedra is more common in temperate and semitropical climates. It commonly results in soft white nodules along the shafts of pubic hair, axillary hair, mustaches, eyebrows, and eyelashes. This is in contrast to black piedra that preferentially affects scalp hair. Black piedra results in the formation of firm nodules along the shaft of the hair. The diagnosis of piedra may be made easily by observation of hyphae on affected hair. Clipping of the affected hair is usually the most effective treatment modality, followed by application of topical antifungals or keratolytics.
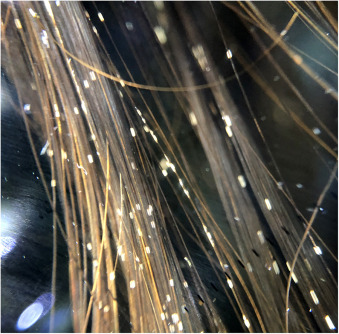
Black piedra is a fungal infection of the hair shafts. It is also known as Trichomycosis nodosa. The fungal elements are attached to the hair shaft to form nodules along the hair shaft. It predominantly affects scalp hair, although involvement of the beard, mustache, and pubic hairs is also known. Black piedra is common in hot and humid countries like South American countries and Southeast Asian countries.
Trichosporon spp. are part of the skin microbiome (oral mucosa and inguinal regions) and are widely distributed in the environment. They can eventually cause soft nodules, known as white piedra, and are also responsible for opportunistic infections in immunosuppressed patients, mainly those with hematologic neoplasia. Pathogenesis of white piedra is unknown. Clinically, it presents with clear, soft and asymptomatic nodules in the naked hair shaft of the pubic hair, axillary hair, beards, mustaches, eyebrows, eyelashes and scalp hair.
Culture of specimens on SDA shows slow-growing brown to reddish black mycelium, which is considered asexual or anamorphic stage of the fungus.
Cutaneous Mycoses
Dermatophytoses or cutaneous mycoses are diseases of the skin, hair, and nail. These infections are caused by a homogeneous group of closely related fungi known as dermatophytes.
Based on their natural habitats, dermatophytes can be classified into following groups:
- Anthropophilic species: These dermatophytes are typically adapted to live on human host. They are transmitted from human to human through fallen hairs, desquamated epithelium, combs, hair brushes, towels, etc. Examples are Trichophyton rubrum, Microsporum audouinii, and Epidermophyton floccosum.
- Zoophilic species: These are the dermatophytes that live on animals and often cause infection in their animal host. These zoophilic species are transmitted from infected animals to humans by direct and indirect contacts with domestic animals. Examples include Trichophyton violaceum and Microsporum canis.
- Geophilic species: These are saprophytic fungi found in soil or in dead organic substances. They occasionally cause infection in humans and animals. Examples are Microsporum gypseum and Trichophyton ajelloi.
Dermatophytes cause chronic infections of the skin often found in the warm humid areas of the body, such as athlete's foot and jock itch. Typical ringworm lesions are circular, which have an inflamed border containing papules and vesicles surrounding a clear area of relatively normal skin
Ringworm can be classified depending on the site affected. These include: Tinea capitis involving scalp, Tinea corporis involving nonhairy skin of the body, Tinea cruris affecting groin, Tinea pedis affecting foot, and Tinea barbae affecting beard areas of face and neck.
Diagnosis
Laboratory diagnosis is based on demonstration of fungal element in clinical specimen by microscopy and confirmation by culture. The specimens include skin scrapings and nail clippings or hair taken from the areas suspected to be infected by dermatophytes. These entire specimens are treated with alkali solution to clear epithelial cells and other debris. Direct microscopy is useful only for diagnosis, while culture is always carried out to identify the specific causative fungal agent.
Treatment
Treatment of dermatophyte infection is carried out by use of local antifungal drugs, such as miconazole, clotrimazole, econazole, etc., or by treatment orally with griseofulvin.
Subcutaneous Mycosis
These are fungal infection associated with development of characteristic lesion in subcutaneous tissue and overlying skin with or without extension to bone and muscle.
Mycetoma
Mycetoma is a slowly progressive, chronic granulomatous infection of skin and subcutaneous tissues with occasional involvement of underlying fascia and bone usually affecting extremities. The condition is characterized by a triad of tumefaction, draining sinuses, and grains or granules. Mycetoma is caused by a number of actinomycetes and filamentous fungi that enter through penetrating injuries resulting from thorn pricks, splinters, etc. It typically affects the lower extremities, but it can occur in almost any region of the body. Microabscesses are formed in subcutaneous tissues surrounded by polymorphonuclear inflammatory reaction. The center of the lesion consists of tangled filaments of these organisms. During the course of infection, microabscesses burst open with the formation of chronic multiple sinuses discharging copious, seropurulent fluid containing granules. The color and consistency of these granules vary depending on the fungi that cause the disease.



Mycetoma is documented worldwide but is common in tropical and subtropical countries. Actinomycetoma accounts nearly for 65% of mycetomas and for 35% of eumycetoma in India.
Diagnosis of Mycetoma
Causative agents can be identified by gross and microscopic examination of grains from exudates, which contain pathognomonic, irregularly shaped, variably colored, 0.5- to 2mm granules. Crushing and culture of these granules provides definitive identification. Exudate specimens may yield multiple bacteria and fungi, some of which are potential causes of superinfections.
Treatment
Treatment of mycetoma may be required for over 10 years. Death may result from bacterial superinfection and sepsis if treatment is neglected. Treatment depends on the causative agent and the extent of the disease.
Treatment is effected using Antibacterial or antifungal drugs. Surgery is required in refractory cases. Limb amputation to prevent potentially fatal severe secondary bacterial infections may be needed in advanced cases.
Chromomycosis
The term chromomycosis includes chromoblastomycosis and phaeohyphomycosis caused by dematiaceous fungi.
Chromoblastomycosis is one of the most prevalent implantation fungal infections, being the most common of the gamut of mycoses caused by melanized or brown-pigmented fungi. CBM is mainly a tropical or subtropical disease that may affect individuals with certain risk factors around the world. The following characteristics are associated with this disease: (i) traumatic inoculation by implantation from an environmental source, leading to an initial cutaneous lesion at the inoculation site;
 (ii) chronic and progressive cutaneous and subcutaneous tissular involvement associated with fibrotic and granulomatous reactions associated with microabscesses and often with tissue proliferation; (iii) a nonprotective T helper type 2 (Th2) immune response with ineffective humoral involvement; and (iv) the presence of muriform (sclerotic) cells embedded in the affected tissue.
(ii) chronic and progressive cutaneous and subcutaneous tissular involvement associated with fibrotic and granulomatous reactions associated with microabscesses and often with tissue proliferation; (iii) a nonprotective T helper type 2 (Th2) immune response with ineffective humoral involvement; and (iv) the presence of muriform (sclerotic) cells embedded in the affected tissue.
The disease has been described worldwide but the prevalence is higher in rural populations in countries with a tropical or subtropical climate, such as Madagascar in Africa and Brazil in South America. Diagnostic techniques are based on direct examination, culture and histopathology. Despite a variety of treatment modalities, which include long courses of antifungals, surgical excision and destructive physical therapies, the disease remains one of the most difficult deep mycotic infections to eradicate.
Phaeohyphomycosis
 is a heterogeneous group of cutaneous diseases caused by various dematiaceous fungi. Phaeohyphomycotic cyst is the most common form described
in this condition.
is a heterogeneous group of cutaneous diseases caused by various dematiaceous fungi. Phaeohyphomycotic cyst is the most common form described
in this condition.
Diagnosis of phaeohyphomycosis is made by demonstration of darkly pigmented, septate hyphae measuring 5-10 µm diameter in tissues. The drug of choice for treatment of chromoblastomycosis is 5-fluorocytosine.
Sporotrichosis

Sporotrichosis is a chronic pyogenic granulomatous lesion of the skin and subcutaneous tissue caused by Sporothrix schenckii. The spore is the infective stage of the fungus. It causes infection primarily on the hand or the forearm through direct contact of the skin by spores. Typically, infection is introduced in skin through a penetration of thorn. In infected tissue, the yeast appears as round, oval, or cigar shaped cells with irregular borders.
Rhinosporidiosis
Rhinosporidiosis is a chronic granulomatous disease caused by Rhinosporidium seeberi. More than 90% of cases are reported from India, Sri Lanka, and South America. The disease is characterized by the development of large friable polyps or wart-like lesion in the nose, conjunctiva, or eye. The lesion is also occasionally seen in ears, larynx, bronchus, urethra, vagina, rectum, and skin.
Treatment of the condition is carried out by surgery or cauterization. Chemotherapy with dapsone is also useful.
Systemic Mycoses
Systemic mycoses are caused by fungi of soil, which are inherently virulent and cause disease in healthy humans. The systemic mycoses include coccidioidomycosis, paracoccidioidomycosis, histoplasmosis, blastomycosis, and cryptococcosis.
Coccidioidomycosis
Valley fever, also called coccidioidomycosis, is an infection caused by the fungus Coccidioides. The fungus is known to live in the soil in the southwestern United States and parts of Mexico and Central and South America. The fungus was also recently found in south-central Washington. People can get Valley fever by breathing in the microscopic fungal spores from the air, although most people who breathe in the spores don't get sick. Usually, people who get sick with Valley fever will get better on their own within weeks to months, but some people will need antifungal medication.
Symptoms of Valley fever include Fatigue (tiredness), Cough, Fever, Shortness of breath, Headache, Night sweats, Muscle aches or joint pain. A rash on upper body or legs may develop. In extremely rare cases, the fungal spores can enter the skin through a cut, wound, or splinter and cause a skin infection.
The fungus that causes Valley fever lives in the soil in the southwestern United States, south-central Washington State, and parts of Mexico and Central and South America.
Laboratory diagnosis of coccidioidomycosis is made by demonstration of spherules containing endospores in (a) sputum, or smears from the lesion stained by calcofluor white and (b) in biopsy material stained by hematoxylin and eosin, silver, or periodic acid-Schiff stains. Culture is the most definitive method for diagnosis. The fungus grows well on Sabouraud's dextrose agar (SDA) and other media producing white and cottony colony within 5 days.
Amphotericin B is the drug of choice for treatment of the condition. However, 3 to 6 months of fluconazole or another type of antifungal medication may also be effective. There are no over-the-counter medications to treat Valley fever.
Paracoccidioidomycosis
Paracoccidioidomycosis is an infection caused by the fungus Paracoccidioides. This fungus lives in parts of Central and South America. Anyone who lives in or visits areas where Paracoccidioides lives can get paracoccidioidomycosis, but it most often affects men who work outdoors in rural areas.
Infection occurs by inhalation of conidia or mycelial fragments. The lungs are the primary site of infection. From this site, the fungus then disseminates to other organs through the venous and lymphatic systems. Cell-mediated immunity (CMI) is the most important defense mechanism in an immunocompetent host. However, most initial infections are subclinical.
Many people who are infected with Paracoccidioides never develop symptoms. 1,2 For people who develop symptoms, paracoccidioidomycosis usually affects the lungs and skin. Other symptoms include: 3,4 Lesions in the mouth and throat, Weight loss, Swollen lymph nodes, Cough, Fever, Shortness of breath, Fatigue, Enlarged liver and spleen. The symptoms of paracoccidioidomycosis can be different for different groups of people.
Laboratory diagnosis depends on demonstration of large, multiple budding yeasts (blastoconidia) in 30% KOH wet mount preparation of sputum.
Itraconazole is the drug of choice for treatment of paracoccidioidomycosis and is effective in 95% of patients. Imidazole is also an effective agent with a cure rate of 85-90%. Amphotericin B is used as a reserve for treatment of severe cases that are refractory to treatment with these drugs.
Histoplasmosis
Histoplasmosis is primarily a disease of reticuloendothelial system caused by an intracellular fungus Histoplasma capsulatum. H. capsulatum is a dimorphic fungus, which occurs in two stages: as a mold in soil and as yeast at body temperature in mammals. Then condition is common in regions around the Ohio and Mississippi River valleys. The fungus also lives in parts of Central and South America, Africa, Asia, and Australia.
People can get histoplasmosis after breathing in the microscopic fungal spores from the air, often after participating in activities that disturb the soil. Although most people who breathe in the spores don't get sick, those who do may have a fever, cough, and fatigue. Many people who get sick will get better on their own without medication. In some people, such as those who have weakened immune systems, the infection can become severe, especially if it spreads from the lungs to other organs.
Most people who are exposed to the fungus never have symptoms. Other people may have symptoms that go away on their own. Histoplasmosis symptoms include Fever, Cough, Fatigue (extreme tiredness), Chills, Headache, Chest pain and Body aches. These symptoms may appear between 3 and 17 days after exposure to the fungal spores.
CMI is key component of host defense against the fungus. T lymphocytes are crucial in limiting the extent of infection. In persons with impaired CMI, Histoplasma species which remained latent in healed granulomas may be reactivated, resulting in histoplasmosis.
Laboratory diagnosis depends on demonstration of oval yeast cells within macrophages in bone marrow aspirates and in tissue biopsy specimens. Biopsy of oropharyngeal ulcers is usually diagnostic.
Amphotericin B is the drug of choice for treatment of disseminated disease. Fluconazole is often recommended for meningitis due to its better penetration of the cerebrospinal fluid (CSF). Asymptomatic or mild condition needs no treatment.
Blastomycosis
Blastomycosis is a granulomatous fungal infection caused by B. dermatitidis. B. dermatitidis is a dimorphic fungus, which occurs in two stages; as mold in soil and as yeast in tissue.
B. dermatitidis infection occurs by inhalation of microconidia found in soil, its natural habitat. Inside the lungs, the conidia are transformed to the yeast phase at body temperature. The thick cell wall of the yeasts offers resistance to phagocytosis and induces expression of blastomyces adhesin 1 (BAD1), an immune-modulating virulence factor on the cell surface. Then, the yeasts replicate and may disseminate through the blood and lymphatics to other organs to cause the disease.
Approximately half of individuals infected with the fungus Blastomyces will show symptoms. The symptoms are often similar to the symptoms of other lung infections, and can include: Fever, Cough, Night sweats, Muscle aches or joint pain, Weight loss, Chest pain and Fatigue (extreme tiredness). In some individuals, particularly those who have weakened immune systems, blastomycosis can spread from the lungs to other parts of the body, such as the skin, bones and joints, and the central nervous system
Blastomycosis is documented from the United States and also from Canada and the African continent. In endemic areas, blastomycosis is a common infection among dogs. It is also reported in horse, cow, cat, bat, and lion.
Amphotericin B and itraconazole are the drugs of choice for treatment of blastomycosis
Cryptococcosis
Cryptococcosis, also called European blastomycosis, is an acute to chronic disease caused by an encapsulated yeast, C. neoformans. Cryptococcosis is the most common life-threatening fungal disease in patients with AIDS. It is the only systemic mycosis frequently documented from India.
C. neoformans is a true yeast. It is an oval and budding cyst and measures 3-6 µm in diameter. The yeast may be single or may have a single budding daughter cell. Within the host and in certain culture media, the yeast is surrounded by a wide polysaccharide capsule. The polysaccharide capsule is composed of mannose, xylose, and glucuronic acid.
Pathogenesis and Immunity
The immune status of the host is the crucial factor in pathogenesis of cryptococcosis. C. neoformans usually causes most serious infections in patients with impaired CMI, including patients with AIDS, patients undergoing corticosteroid treatment, patients undergoing organ transplantation, patients with reticuloendothelial malignancy, and patients with sarcoidosis. C. neoformans is primarily transmitted by inhalation After inhalation, the yeasts are deposited into the pulmonary alveoli, in which they are phagocytosed by alveolar macrophages. However, the antiphagocytic properties of the capsule prevent recognition of the yeast by phagocytes and inhibit leukocyte migration into the area of fungal replication.
C. neoformans causes three forms of cryptococcosis;
(a) pulmonary cryptococcosis occurs in immunocompetent hosts and in immunocompromised hosts
(b) CNS cryptococcosis,
(c) disseminated nonpulmonary non-CNS cryptococcosis.
Diagnosis
C. neoformans is distributed worldwide. The incidence of cryptococcosis is increasing and now it represents a major life threatening fungal infection in patients with AIDS.
Treatment
Amphotericin B is the drug of choice for initial therapy in meningitis or other disseminated infections caused by C. neoformans. Amphotericin B may be used alone or in combination with flucytosine.
Opportunistic Fungal Infections
The opportunistic fungi usually cause infections in persons with impaired host defense, but do not cause disease in most of the immunocompetent hosts. Since these fungi become pathogens in individuals with impaired immunity by taking advantage of the host's debilitated conditions, they are called opportunistic fungi. Most opportunistic infections are caused by Candida albicans, Aspergillus spp., Penicillium marneffei, and various Zygomycetes.
Candidiasis
Candidiasis is a fungal infection caused by a yeast (a type of fungus) called Candida. Some species of Candida can cause infection in people; the most common is Candida albicans. Candida normally lives on the skin and inside the body, in places such as the mouth, throat, gut, and vagina, without causing any problems. Candida can cause infections if it grows out of control or if it enters deep into the body (for example, the bloodstream or internal organs like the kidney, heart, or brain). Candida shows colonization at these sites in more than 80% of healthy people. The organism, however, is rarely present on the surface of normal human skin, except occasionally from certain intertriginous area, such as the groin
Pathogenesis of Candida infection
Under certain conditions, Candida gains access to systemic circulation from the oropharynx of the gastrointestinal tract. In immunocompromised hosts, Candida may disseminate to many organs, such as lung, spleen, liver, heart, and brain. Candida causes a wide spectrum of clinical illnesses.
- Cutaneous candidiasis: In immunocompetent host, candida can cause infection of any warm and moist part of the body exposed to environment. It causes infection of the nail, rectum, and other skin folds.
- Mucocutaneous candidiasis: Mucocutaneous candidiasis (thrush, perianal disease, etc.) is the most common manifestation of candidiasis, but usually does not cause any mortality. In patients with advanced immunodeficiency due to HIV infection, Candida species can cause severe oropharyngeal and esophageal candidiasis that result in poor intake of food, leading to malnutrition, wasting, and early death.
- Chronic mucocutaneous candidiasis: This syndrome is characterized by chronic, treatment-resistant, superficial Candida infection of the skin, nails, and oropharynx.
- Systemic candidiasis: These include endocarditis, gastrointestinal tract candidiasis, respiratory tract candidiasis, genitourinary candidiasis, and hepatosplenic candidiasis.
- Disseminated candidiasis: This is increasingly becoming a problem in patients with serious hematologic malignancies that are treated with immunosuppressive drugs for over a long period of time. In this condition, Candida usually spreads through the circulation and involves many organs, such as lungs, spleen, kidney, liver, heart, and brain
Host Immunity
Both cell-mediated and humoral antibodies confer protection against Candida in healthy adults. Cell-mediated immunity (CMI) is, however, most important.
Epidemiology
Candida species is distributed worldwide. In recent times, Candida species have replaced Cryptococcus species as the most common fungi affecting the CNS of immunocompromised patients worldwide.
Diagnosis
Specimen include exudates or tissues for microscopy obtained from skin or nails examined by microscope for demonstration of pseudohyphae or budding yeast cells of Candida. Gram-stained smear of the exudates or tissue shows Gram positive, oval, budding yeast and pseudohyphae.
Treatment
Antifungal therapy forms the mainstay of treatment of the infections caused by Candida. These agents include azoles ( fluconazole, triazole, ketoconazole), nystatin, and amphotericin B.
For prevention, antifungal prophylaxis is indicated for patients with invasive candidiasis who are at high risk of developing invasive candidiasis. There is no vaccine available against candidia
Aspergillosis
Aspergillosis is an infection caused by Aspergillus, a common mold that lives indoors and outdoors. Most people breathe in Aspergillus spores every day without getting sick. However, people with weakened immune systems or lung diseases are at a higher risk of developing health problems due to Aspergillus. The types of health problems caused by Aspergillus include allergic reactions, lung infections, and infections in other organs.
Aspergillus species are identified by their morphological features, the pattern of conidiophore development, and the color of the conidia. The presence of septate hyphae that branch at 45o angles is the typical feature of Aspergillus species hyphae. The hyphae in tissues are best demonstrated with silver stains. The walls of the hyphae are more or less parallel, unlike those of Mucor and Rhizopus, which are more or less irregular.
Pathogenesis
Types of aspergillosis
Allergic bronchopulmonary aspergillosis (ABPA): Occurs when Aspergillus causes inflammation in the lungs and allergy symptoms such as coughing and wheezing, but doesn't cause an infection.
Allergic Aspergillus sinusitis: Occurs when Aspergillus causes inflammation in the sinuses and symptoms of a sinus infection (drainage, stuffiness, headache) but doesn't cause an infection.
Azole-Resistant Aspergillus fumigatus: Occurs when one species of Aspergillus, A. fumigatus, becomes resistant to certain medicines used to treat it. Patients with resistant infections might not get better with treatment.
Aspergilloma: Occurs when a ball of Aspergillus grows in the lungs or sinuses, but usually does not spread to other parts of the body.4 Aspergilloma is also called a "fungus ball."
Chronic pulmonary aspergillosis: Occurs when Aspergillus infection causes cavities in the lungs, and can be a long-term (3 months or more) condition. One or more fungal balls (aspergillomas) may also be present in the lungs.
Invasive aspergillosis: Occurs when Aspergillus causes a serious infection, and usually affects people who have weakened immune systems, such as people who have had an organ transplant or a stem cell transplant. Invasive aspergillosis most commonly affects the lungs, but it can also spread to other parts of the body.
Cutaneous (skin) aspergillosis: Occurs when Aspergillus enters the body through a break in the skin (for example, after surgery or a burn wound) and causes infection, usually in people who have weakened immune systems. Cutaneous aspergillosis can also occur if invasive aspergillosis spreads to the skin from somewhere else in the body, such as the lungs.
Epidemiology
Unlike Candida, Aspergillus spp do not form part of the normal flora in humans. Various clinical manifestations of Aspergillus infection have been documented worldwide. The incidence of allergic bronchopulmonary aspergillosis has been increasingly documented in people with asthma in United Kingdom.
Diagnosis
Laboratory diagnosis of invasive aspergillosis or chronic necrotizing aspergillus pneumonia depends on demonstration of Aspergillus in tissue by direct microscopy and culture.
Treatment
Amphotericin B is most frequently used for treatment of invasive aspergillosis. However, the outcome of treatment is not satisfactory. Caspofungin is an alternative drug given to patients who do not respond to amphotericin B.
Zygomycosis
Zygomycosis, also known as mucormycosis or phycomycosis, is an infection caused by saprophytic molds, such as Mucor, Rhizopus, and Absidia. These fungi are ubiquitous in the environment and generally saprophytic. They rarely cause disease in immunocompetent hosts, but they are the third most frequent cause of invasive fungal infection in immunocompromised patients
Most of the infections produced by Zygomycetes are acute and are usually fatal despite early diagnosis and treatment. The agents of zygomycosis are transmitted by air, through their asexual spores. In humans, they invade tissues of patients with reduced host defense. From there, they enter the blood vessels and proliferate in the walls of blood vessels particularly paranasal sinuses, lungs, or intestines. This results in infarction and necrosis of tissues distal to blocked vessels
Clinical diagnosis of the zygomycosis is frequently difficult. It requires a high degree of suspicion and a host with appropriate risk factors. Laboratory diagnosis is by microscopy, culture, and histopathology.
Pneumocystosis
Pneumocystis jiroveci, previously known as Pneumocystis carinii, is the causative agent of P. carinii pneumonia (PCP). PCP is the most common opportunistic infection in HIV-infected patients.
PCP spreads from person to person through the air (inhalation). Some healthy adults can carry the Pneumocystis fungus in their lungs without having symptoms, and it can spread to other people, including those with weakened immune systems. Many people are exposed to Pneumocystis as children, but they likely do not get sick because their immune systems prevent the fungus from causing an infection. In the past, scientists believed that people who had been exposed to Pneumocystis as children could later develop PCP from that childhood infection if their immune systems became weakened. However, it is more likely that people get PCP after being exposed to someone else who has PCP or who is carrying the fungus in their lungs without having symptoms.
In symptomatic cases, sudden onset of fever, nonproductive cough, dyspnea, and tachypnea are typical manifestations. Bilateral rales and ronchi are present. Extrapulmonary manifestations are rare. It occurs in AIDS patients during their advanced stage.
Epidemiology
Pneumocystis first came to attention when it was found to cause interstitial pneumonia in Central and Eastern Europe during World War II in severely malnourished and premature infants.
PCP causes a mortality of 10-20% in patients with HIV depending on the stage of the disease. It also causes a considerable degree of mortality and morbidity in non-HIV patients.
Diagnosis
Chest radiographs in most patients show diffuse bilateral infiltrates extending from the perihilar region. Patchy asymmetric infiltrates and pneumatoceles are less common finding.
Treatment and Prevention
P. jiroveci, although considered a fungus, does not respond to treatment with antifungal agents. A combination of trimethoprim and sulfamethoxazole is the drug of choice for treatment of PCP. Pentamidine and atovaquone are alternative drugs.
Chemoprophylaxis with trimethoprim and sulfamethoxazole or aerosolized pentamidine is useful for prevention of infection in patients with CD4 counts below 200/µL.
Penicilliosis
Penicillium species rarely cause opportunistic infections in humans. The Penicillium species are identified by their typical morphology, culture characteristics on the SDA medium, and microscopy.
P. marneffei is the only dimorphic fungus in the genus Penicillium known to cause opportunistic infection.
P. marneffei is the only dimorphic fungus in the genus Penicillium. It has been reported as an important opportunistic pathogen in AIDS patients. The fungus causes tuberculosis-like disease in patients with AIDS in Southeast Asian countries like Thailand. Few case reports have also been documented from India.
P. marneffei is widely distributed in the nature. Its natural habitat is soil. The fungus infects no mammals other than humans and bamboo rat. Fungus is found in feces of rats and also in burrows made by the rats in the soil. The infection is transmitted by inhalation of conidia, direct inoculation of the skin, and rarely, by ingestion of infected rats. The condition is more common in rainy season, in rural areas. Cell-mediated immunodeficiency, steroid treatment, and HIV infection are predisposing factors.
Pseudoallescheria boydii Infection
Pseudoallescheria boydii is a mold that causes an opportunistic infection in immunocompromised persons, such as patients with HIV. It causes a disease, which clinically resembles aspergillosis. The diagnosis is made by demonstration of septate hyphae in tissue that resemble with those of Aspergillus. It can be differentiated from Aspergillus by culture on SDA medium. On culture, P. boydii produces pear-shaped conidia.
Fusarium solani Infection
Fusarium solani is a mold that causes disease primarily in neutropenic patients. It resembles Aspergillus in that it is a mold with aseptate hyphae, which tends to invade blood vessels. Fever associated with lesions in the skin is the common clinical presentation. The fungus differs from Aspergillus by culture in which it produces banana-shaped conidia.